Content
Module 4: Medications
Introduction
This module covers the medications used during an awake bronchoscopic intubation – anti-sialogogues, local anesthetics, vasoconstrictors and sedatives. Choosing and delivering medication for an awake bronchoscopic intubation follows multiple RULES OF 3. Look out for the icon in the text below.
There are groups of medications that need to be considered:
- Anti-sialagogues
- Local Anesthetics (+/- vasoconstrictor)
- Sedatives
Anti-sialagogues
There are reasons for using an anti-sialagogue:
- Improved view due to reduced secretions
- Increased effectiveness of the local anesthetic. Secretions dilute the local anesthetic, create a barrier between mucosa and local anesthetic and carry the local anesthetic away from the site of intended action. For all of these reasons, reduced secretions = better topicalization.
- Reduces the risk that secretions will cause cough and/or laryngospasm
Any anticholinergic agent can be used (atropine, scopolamine or glycopyrrolate) however glycopyrrolate has several advantages including lack of central nervous system effects (it does not cross the blood brain barrier) and less tachycardia than atropine. A dose of 3 – 4 µg/kg is suggested, or for most adults 0.2mg. If the IM route is chosen, it should be given at least 15 mins before.
If dexmedetomidine is the chosen sedative, there is no need for an additional anti-sialagogue.
Vasoconstrictors
When choosing the nasal route a vasoconstrictor should be used to reduce the risk of epistaxis. These agents primarily cause vasoconstriction of the nasal mucosa by acting as alpha 1 agonists.
Options include:
- using cocaine (generally 4%) as your chosen local anesthetic (inherent vasoconstrictor properties)
- oxymetazoline 0.05%
- xylometazoline 0.1% (Otrivin)
- phenylephrine 0.5% (or co-phenylcaine – Lidocaine 5% and phenylephrine 0.5%)
Local Anesthetics
Once again, there are decisions to be made.
Decision 1: Which agent to choose?
- Lidocaine: Readily available, comes in many strengths and formulations, rapid onset and relatively low cardiac toxicity.
- Cocaine: Inherent vasoconstrictor properties. Potential adverse effects include tachycardia, hypertension and arrhythmias. More restricted availability than lidocaine. Maximum dose of 1 - 3mg/kg.
Decision 2: What dose to use?
- Suggested maximum dose of lidocaine = 5mg/kg without adrenaline and 7mg/kg with.
- Traditionally much higher doses (up to 9mg/kg) have been used safely for airway topicalization, since much of what is delivered is either swallowed or lost to the atmosphere and therefore not absorbed. However, we should also consider that plasma levels rise rapidly after topical application of local anesthetic to the respiratory tract.
- Early signs of local anesthetic toxicity include peri-oral numbness/tingling, light-headedness, metallic taste and visual/auditory disturbances.
- Calculate maximum dose of local anesthetic based on patient body weight (lean body weight) and divide this total volume among the different areas to be topicalized.
Decision 3: What technique to use?
There are areas that need to be anesthetized:
- Nasal passage and nasopharynx
Some suggest preparing the nose even if the oral route is planned due to passive leak of local anesthetic into the oropharynx, and, in the case of difficult oral intubation, the nose is already prepared
Techniques for anaesthetizing the nasal passage include:
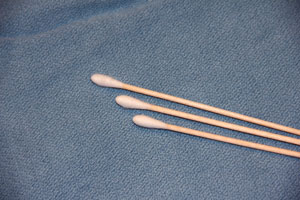
- Cotton tipped swabs soaked in local anesthetic slowly advanced deeper into nasal cavity
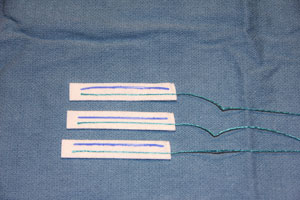
- 'Neuro patties' soaked in local anesthetic inserted into the floor of the nose and allowed to sit for 5 – 10 mins
- Nasal mucosal atomization device (MADTM Wolf Tory Medical)
_sm.jpg)
- Nasopharyngeal airway coated in local anesthetic gel (prelubricates, anaesthetizes and ensures nasal patency)
- Cotton tipped swabs soaked in local anesthetic slowly advanced deeper into nasal cavity
- Oropharynx
Techniques for anaesthetizing the oropharynx include:
- Nebulization of local anesthesia
- Atomization of local anesthesia using a 3 way stopcock and oxygen tubing
_sm.jpg)
- Oral MAD device
_sm.jpg)
- Gargling: Several ml of local anesthetic solution gargled by the patient with the excess expectorated
- "Drummonds toothpaste method": local anesthetic jelly applied to the base of the tongue and anterior tonsillar pillars via a tongue depressor; patient holds the tongue depressor in their mouth like a lollypop but instructed not to swallow; local anesthetic 'melts' and runs down the back of the hypopharynx
- "Pacey's Paste": A 50:50 mixture of 2% lidocaine solution with 2% lidocaine jelly is created with the use of a 3 way stopcock. The resulting mixture is a sticky, viscous fluid that is dribbled onto the back of the tongue.
_sm.jpg)
- Various nerve blocks can also be used (See the advanced knowledge portion of this module)
- Larynx and Trachea
Techniques for anaesthetizing the larynx and trachea include:
- Steady trickling of lidocaine onto the posterior portion of the tongue while the tongue is manually pulled forward (this is key as it prevents proper swallowing and facilitates aspiration)
_sm.jpg)
- Trans-tracheal injection of 2 – 3ml lidocaine via the cricothyroid membrane using a cannula (the needle is removed prior to injection, to prevent airway injury when the patient coughs
- "Spray as you go" via the working port of the bronchoscope or an epidural catheter through the working port of the scope, with aliquots delivered to the epiglottis, vocal cords then subglottic area
- Various nerve blocks can also be used (See the advanced knowledge portion of this module)
- Steady trickling of lidocaine onto the posterior portion of the tongue while the tongue is manually pulled forward (this is key as it prevents proper swallowing and facilitates aspiration)
Sedatives
The ideal sedative for awake bronchoscopic intubation will provide:
- patient comfort and co-operation
- anxiolysis
- amnesia
- attenuated airway reflexes, anti-tussive
- stable hemodynamics
- maintenance of a patent airway with spontaneous ventilation
The available agents include:
- Benzodiazepines (midazolam)
- Propofol
- Alpha 2 agonists (clonidine and dexmedetomidine)
- Opioids (fentanyl, remifentanil)
- Ketamine
For all agents, careful titration is essential and, where applicable, reversal agents should be readily accessible (naloxone, flumazenil). When a combination of agents is used, the effect may be synergistic so extreme caution is required.
| Dexmedetomidine | |
| DOSE | Loading dose of 1µg/kg over 10 mins (0.5µg/kg for age > 65) then 0.2 – 1.0µg/kg/hour. |
| PREPARATION | 200µg (2 mL) in 48ml saline to make a 50ml solution. Gives a concentration of 4 µg/ml. |
| ACTION | Highly selective alpha 2 agonist. Sedative effect is due to activation of the post synaptic alpha 2 receptors in the locus coeruleus. |
| CLINICAL EFFECTS | Sedative. Analgesic. Anxiolytic and Antisialogogue. Onset of sedation approx 10 – 15 mins after the start of the infusion. |
| ADVANTAGES | Minimal respiratory depression, no need for additional anti-sialagogue. |
| ADVERSE EFFECTS | Hypotension, bradycardia, sinus arrest, dry mouth. Potential for hypertension initially if high dose infusion or rapid bolus – due to stimulation of peripheral alpha 2 receptors. |
| Remifentanil | |
| DOSE | Infusion 0.02 – 0.2µg/kg/min. Alternatively, loading dose of 0.5-0.7µg/kg and infusion of 0.05-0.1 µg /kg/min. If available, can use the minto TCI protocol in a range of 2 – 5ng/ml. |
| ACTION | Opioid agonist |
| CLINICAL EFFECTS | Analgesia, sedation. |
| ADVANTAGES | Analgesia and depression of airway reflexes, including coughing. Rapidly titratable. Antagonist available. |
| ADVERSE EFFECTS | Respiratory depression, susceptible to aspiration due to depression of reflexes, bradycardia, hypotension, no amnesia therefore higher incidence of recall. |
| Ketamine | |
| DOSE | Bolus 10 – 20mg then 20mg/hr (0.2 – 0.4mg/kg/hr). |
| ACTION | NMDA receptor antagonist. |
| CLINICAL EFFECTS | Dissociative state, analgesia, sedation. |
| ADVANTAGES | Useful in conjunction with dexmedetomidine as it balances the bradycardia and hypotension. Bronchodilation, sympathomimetic effects without apnea. |
| ADVERSE EFFECTS | Excessive secretions, hallucinations. |
Continue to: Module 4: Advanced Knowledge

