Risks
As with all surgical procedures, robotic hysterectomy has some risks, but the chance of any of these happening is very low.


Infection
Before we start, we clean the skin with a special solution to prevent infection. Antibiotics are given as well. Common sites for infection include:
- Bladder (urinary tract)
- Skin incisions
- Vagina
- Pelvis
Bleeding
Most patients will have a small amount of bleeding during and after the procedure. If there is more bleeding than expected, your surgeon might use medications to help control the bleeding. Rarely, a blood transfusion may be needed. Prior to surgery, all patients are asked to indicate whether or not they would accept a blood transfusion in life saving circumstances.
Bleeding (continued)
It is important to make sure that your red blood cell counts (hemoglobin) are normal before surgery. Low hemoglobin is referred to as anemia. Iron supplements and/or medications to decrease vaginal bleeding can be used to increase your blood counts. Some patients may develop anemia after surgery, which may also require iron treatment.
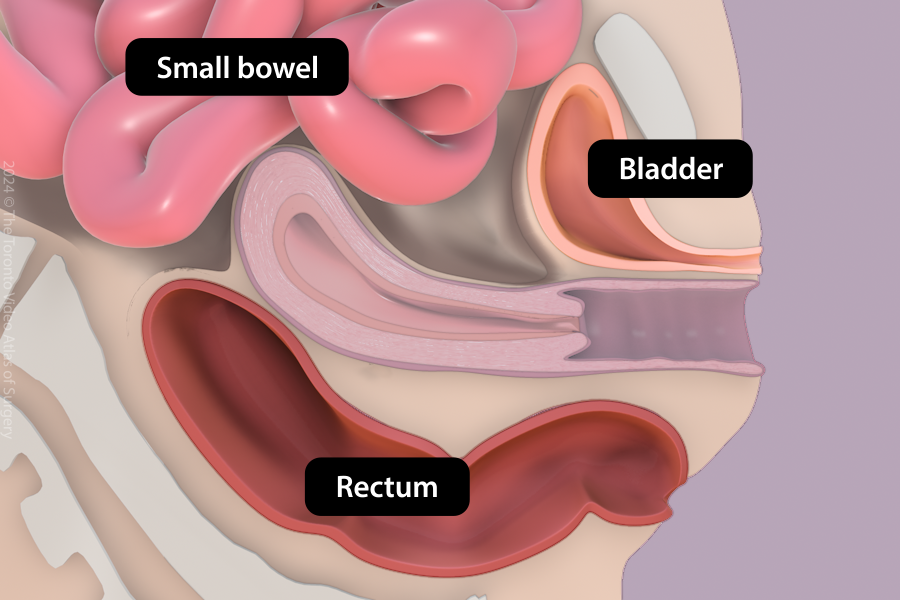
Injury to abdominal organs
There are many important structures in the abdomen and pelvis, for example, the bowel, bladder, ureters, and blood vessels. It is rare that these structures are injured during surgery. This risk is slightly higher in patients who have endometriosis and/or previous abdominal surgeries. If there is an injury, we will repair it and call another specialized doctor, if needed. In some cases, a second procedure may be needed to fix it.
Risk of injury is specifically increased in patients affected by obesity. For these reasons, these patients may have an increased risk of admission to the intensive care unit (ICU) and death.
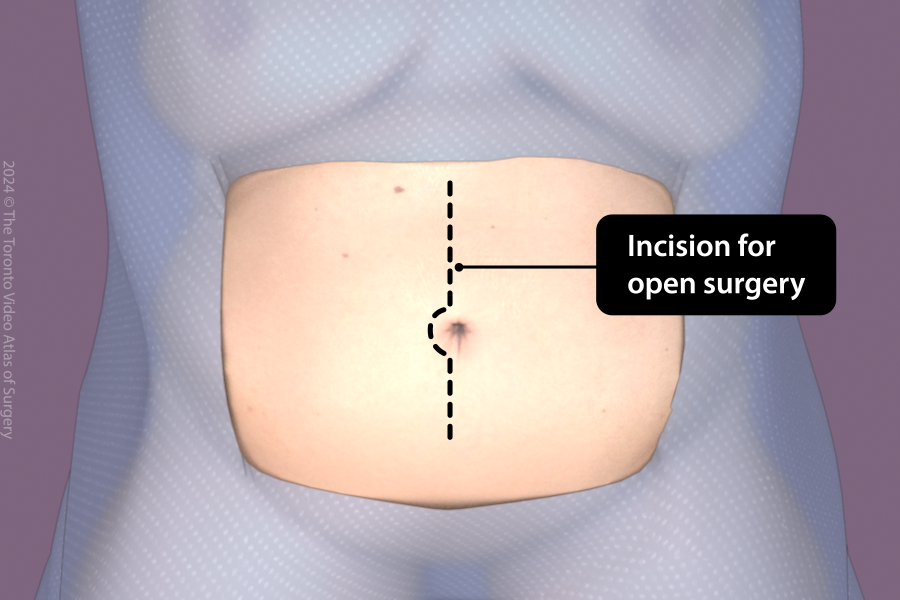
Conversion to open surgery (Laparotomy)
In very rare cases, the surgery cannot be safely completed robotically and a larger incision is made on the abdomen, either vertically or horizontally. If this happens, you may require a longer hospital stay and recovery.
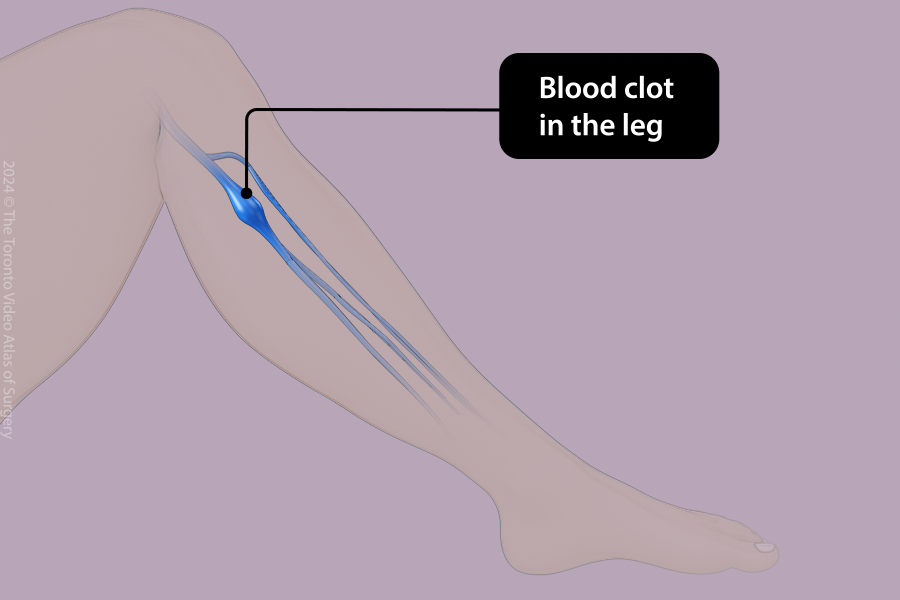
Blood clot
The risk of a blood clot (venous thromboembolism or VTE) in your legs or lungs is increased after surgery but is still uncommon. Risk factors for blood clots include: clotting disorders, obesity, pregnancy, immobility, cancer, or having a previous history of blood clots. As such, you will be encouraged to walk often and early after surgery to minimize this risk. While you are in hospital, you will receive specialized leg stockings (compression devices) and/or blood thinners (medications to prevent blood clots). Blood thinners may be continued after surgery for several weeks.
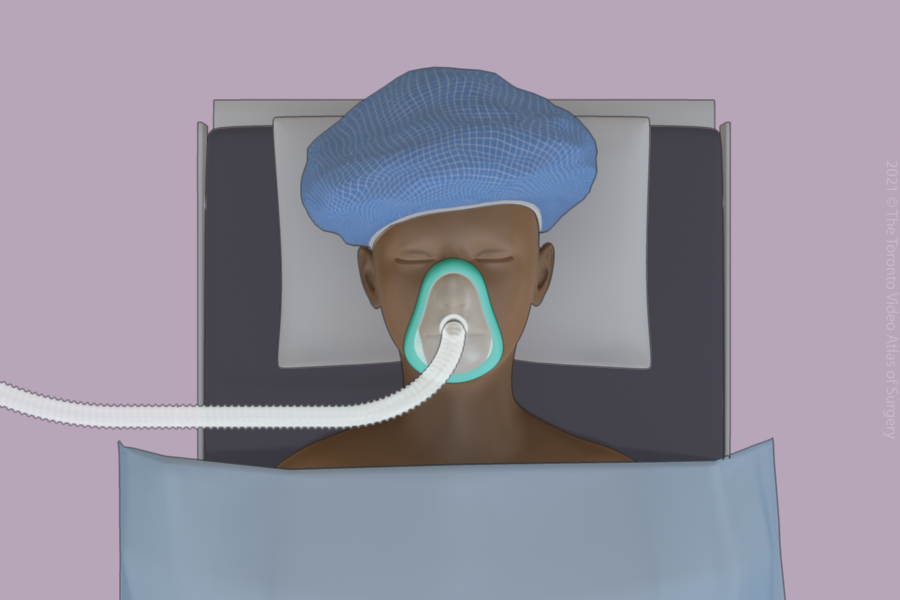
Anesthesia
You must be asleep for the procedure (general anesthesia) to allow the surgeon to see and operate safely. General anesthesia is safe and the anesthetist will talk to you about your specific risks before the surgery. Your anesthetist will carefully monitor you throughout the surgery.
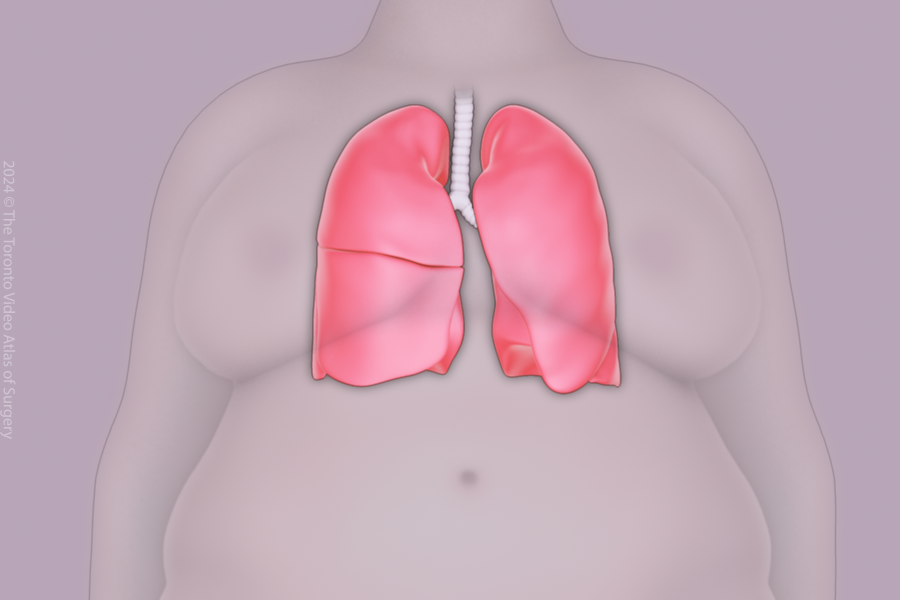
Breathing issues
Anesthesia can temporarily affect lung function, increasing the risk of breathing problems after surgery. The healthcare team will closely monitor your breathing and provide support like specialized breathing exercises/devices as needed to help open up your lungs.
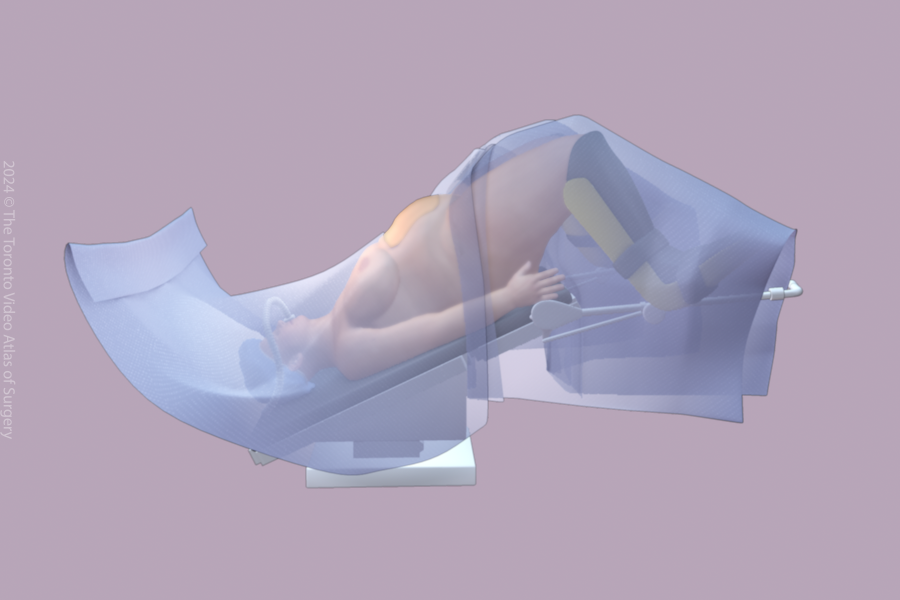
Nerve injury
In some circumstances, there can be injuries to your nerves (shoulders or legs) from pressure from being in the same position for a long time during the surgery. We will position you with padding and supports to decrease this risk. If this happens, you may require a longer admission to hospital and recovery.