What to expect
Preparing for your hysteroscopy
- Before you come in
- Your team
- Anesthesia
- Surgical checklist
- Preparation
- The procedure
- Recovery and discharge


Diet
STOP eating solids or drinking non-clear fluids 8 hours before (eg. milk, orange juice, coffee with milk)
STOP drinking clear fluids 3 hours before (eg. water, clear juice)

Hair removal is not required

Nail polish is permitted

Arrival
Usually 2 hours before your surgery time.

Clothing
You will be asked to change into a hospital gown once you arrive.

Nursing care
An intravenous (IV) line will be placed in your hand to give you fluids and medications during your procedure.

In preparation for your procedure, you will be brought to the operating room where you will meet several members of the medical team involved in your surgery, including:

The anaesthetist
Who will be putting you to sleep or sedating you for the procedure.

The surgeon
Who will be performing your hysteroscopy.

The surgical assistant
There may be a surgical assistant who is a fellow, resident, or another doctor.

The nursing team
There may be an additional nurse who will assist with the surgery.
Some hospitals also have students in any of these roles who may be assisting or observing the procedure.
The size of your team does not necessarily reflect the complexity of your case. Rather, there are many hands to take good care of you!

General anesthetic
You may be put to sleep for this procedure.

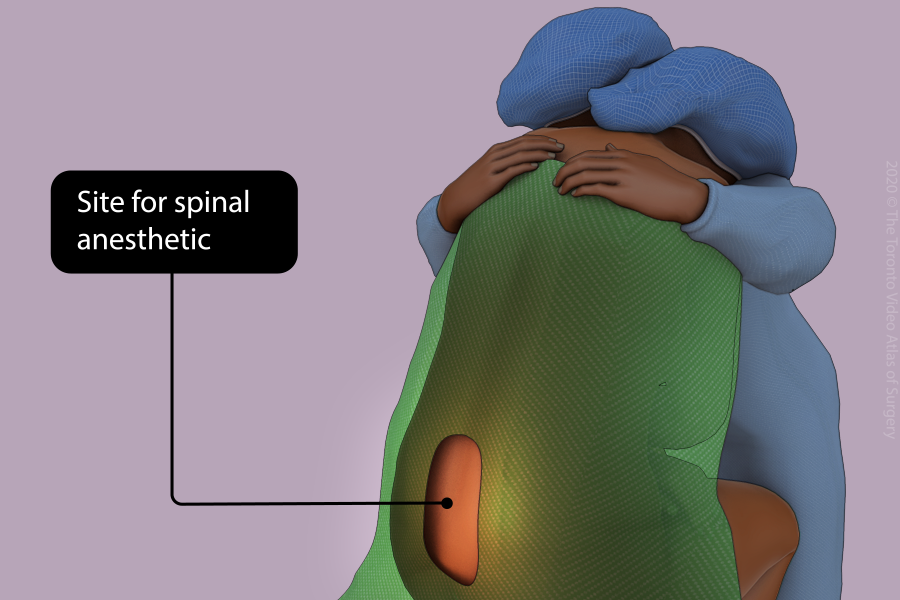
Spinal anesthetic
You may be awake but numb from the waist down using freezing in your back.

Sedation
You may be awake but given medications through the intravenous tube in your hand or arm to make you comfortable during the procedure.


A surgical safety checklist will be performed prior to starting the surgery. The surgical safety checklist is important to make sure that everyone in the operating room (including you!) agrees with the surgical plan.

It is also an opportunity for you to ask any last minute questions. You will be asked to confirm your name and birthdate and the surgeon will review the procedure out loud.

The anesthetist and the nursing team will review your history and ensure that all the equipment is in the room.


Once you are comfortable (or asleep) you will be positioned, lying on your back with your feet supported in stirrups.

The vagina and cervix are then cleaned with a special solution to prevent infection.

Your body will be covered by a sterile sheet to protect you during the surgery.

Sometimes a small tube (Foley catheter) will be placed inside your bladder to keep it empty for the procedure. This is usually removed after the surgery.

A speculum is usually placed inside the vagina in order to see your cervix, just like during a pap test.

The hysteroscope is inserted into your vagina, through the cervix, and into the uterus.

Once inside the uterus, the hysteroscope releases fluid to gently expand the uterine cavity and allow your doctor to see the entire lining of the uterus (endometrium).

At the top of the uterus, the opening to the fallopian tubes (tubal ostia) can be seen as two small holes on the top left and right of the uterus.

If there are polyps or fibroids, an instrument attached to the hysteroscope can be used to remove them.

Anything that is removed will be sent to the pathologist to look at under the microscope.


After your procedure, you will be transferred to the recovery room and monitored closely until all medications wear off.

You will be encouraged to drink fluids and walk as soon as you feel ready.

Non-prescription pain medications like acetaminophen (Tylenol) and ibuprofen (Advil) or naproxen (Aleve) are usually enough for good pain control. You should not need a prescription for pain medication after this procedure.