Patient Learning: SURGICAL TREATMENT for ULCERATIVE COLITIS
INTRODUCTION
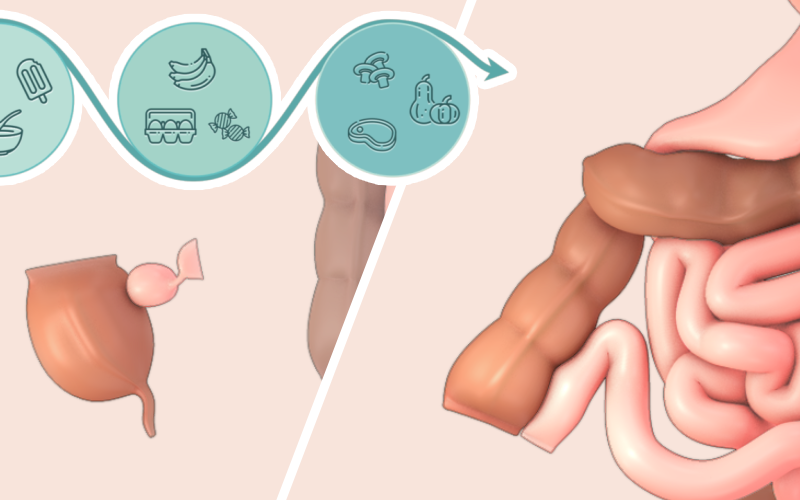
- 00:38 Anatomy
- 02:08 Symptoms
- 02:44 Surgical options
BEFORE SURGERY
- 04:03 Preparing for surgery
- 05:37 Entering any surgery
SURGERY
- 06:30 Types of surgeries
- 08:07 Possible pathways
- 11:46 Risks
AFTER SURGERY
- 12:53 Recovery in the hospital
- 13:58 Recovery at home
- 15:19 Long-term management
SPECIAL ACKNOWLEDGEMENT
This video was a collaboration project with Dr. Mantaj Brar, Dr. Vivian Huang and Ms. Gajuna Mathiyal at the Centre for Inflammatory Bowel Disease, Mount Sinai Hospital.
SURGICAL OPTIONS
** Please buy pro to create nested accordion** id="16849"]
INFORMATION FOR PATIENTS AND FAMILY
- Surgical treatment options for patients with ulcerative colitis disease will result in one of two possible endpoints:
- a permanent stoma,
- or a J-pouch. The J pouch is a surgically-made reservoir to replace the rectum that is removed to relieve your symptoms from ulcerative colitis. A J pouch allows for patients to avoid the need for a stoma.
- This video will cover:
- the anatomy involved in your disease and surgical treatment,
- what you need to know about surgeries for ulcerative colitis,
- and what to expect before, during, and after surgery.
SURGICAL RISKS
With any surgery, there are risks.
- There is a small chance of infection at the surgical incision, and a small chance of bleeding during the surgery that would require a blood transfusion.
- There is also a small chance of a leak from one of the surgical connection sites. If this occurs, you will need intravenous antibiotics, and may require an additional surgery, depending on the severity of the leak.
- There is a risk of scar tissue after surgery, and this may cause bowel obstructions in the future. Bowel obstructions usually resolve without the need of further surgery.
- For female patients, J pouch surgery can present a risk of infertility, due to the surgical sites being in close proximity to the female reproductive organs, and the possibility of scar tissue forming around the fallopian tubes.
- There is a small risk of sexual dysfunction in both men and women after rectal surgery.
- Patients may experience inflammation of the J pouch, known as “pouchitis”. If this occurs, it can be treated with antibiotics most of the time. In instances of persistent pouchitis, an additional surgery may be required to remove the pouch and replace it with a stoma.
Because the symptoms of J-pouch related complications are not always specific and may overlap, it is very important you report any symptoms to your doctor as soon as possible. Early intervention is key to a successful resolution.
LIFE AFTER SURGERY
- Throughout your recovery, keeping a journal of your weight, diet, medications, mood, and any questions or concerns, will be helpful for your follow up appointments. Just as before surgery, it will be important to maintain a healthy weight after surgery. It is also important to follow a strict diet with a stoma to avoid obstructions.
- You are cleared to start doing regular cardiovascular exercise as early as 1 week after a surgery if you feel up to it, and return to normal activities within 4-6 weeks, apart from lifting or strenuous abdominal exercises.
- When your surgical treatment ends with a stoma, you will have new routines for care and management. Because the stoma has no sphincter muscle like the anus does, there is no voluntary control over the passage of stool, so an external appliance must be worn at all times.
- After ileostomy surgery, the stoma may take 1-4 days to start functioning, after which most patients will need to empty the appliance (ostomy bag) 4-6 times a day.
- After a surgery that creates a diverting ileostomy (also referred to as a "loop ileostomy"), there is a higher risk of dehydration. This type of stoma is more challenging to manage than an “end ileostomy”, because it doesn’t stick out as far from the skin. With either type of stoma, mucus secretions from the anus soon after surgery are normal, even though you won’t be passing stool.
- Unlike the rectum that was removed, the J pouch can not contract to squeeze out stool, it instead empties by gravity, so passing stool can take longer than what you’ve been used to.
- J pouch function will improve over time, at 6 to 9 months post-surgery most patients experience 6-8 bowel movements a day or fewer, their stool reaches a pasty consistency, they have on average 1-2 bowel movements per night, and do not experience urgency or incontinence.
GLOSSARY of MEDICAL TERMS
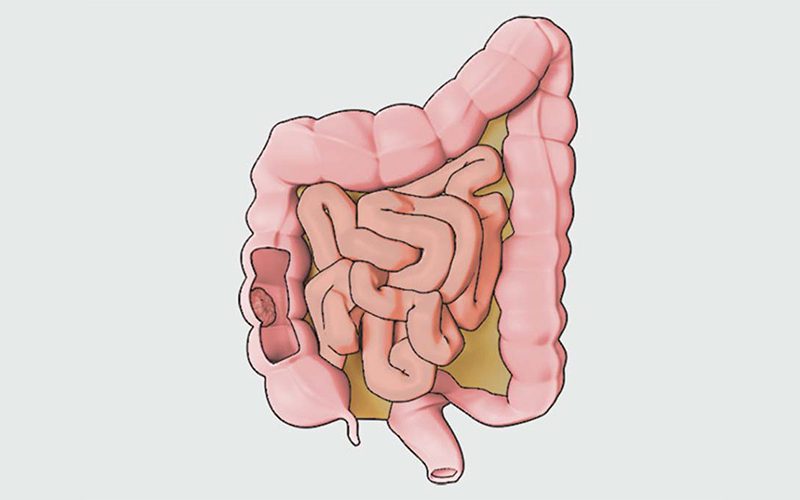
- Colectomy : a surgery to remove part (subtotal) or all (total) of your colon
- Comorbidity : a situation where a patient has more than one disease or condition at the same time
- Ileostomy : a surgery to bring your bowel to the skin through an opening made in the abdominal wall. There are two main types of ileostomies you should know about:
- “End” ileostomy : is when the small bowel terminates at the stoma. This is the result of a total or subtotal colectomy
- “Diverting” or “Loop” ileostomy : is when the small bowel has been partially cut open to expose two openings, but only one is evacuating stool. This type of ileostomy follows the construction of a J pouch and is temporary, allowing the J pouch time to heal
- Laparoscopic : also referred to as minimally invasive or “keyhole” surgery, a type of surgery where instruments are inserted through several small incisions as opposed to one large opening
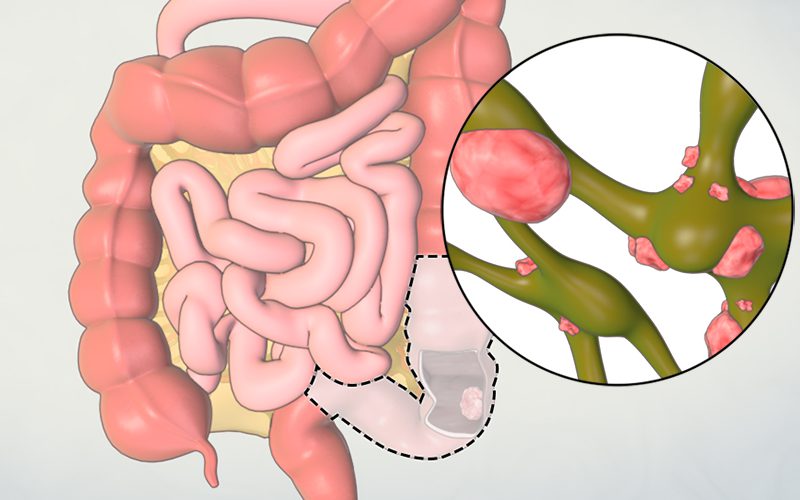
- Left-sided colitis : when ulcerative colitis involves the rectum and sigmoid colon, with or without the descending colon
- Pancolitis : when ulcerative colitis involves the rectum, sigmoid colon, descending colon, and any portion of the colon further upstream to the descending colon
- Proctitis : when ulcerative colitis is limited to the rectum
- Proctocolectomy : a surgery to remove the entire colon including the rectum and anus
- Stoma : the exposed portion of bowel that evacuates stool following ileostomy surgery
- Ulcerative Colitis : one type of Inflammatory Bowel Disease (IBD) that affects the inner lining, or mucosa, of your colon (i.e. large intestine, large bowel)
USEFUL LINKS