Fluid restriction is a key component of treating heart failure. Normally, the body is able to deal with extra fluid by excreting it as urine. Patients with heart failure lose this ability to excrete extra fluid, and therefore it accumulates in the body.
When you drink too much fluid, your heart has to work harder to pump the excess fluid around your body. Extra fluid accumulates slowly, but over time, large amounts can build up. Not all of this extra fluid stays in the blood vessels. Some seep out into the tissues in your ankles and legs, causing swelling. The fluid may also accumulate in your lungs, making it difficult to breathe, particularly when lying flat.
What is Water Weight?
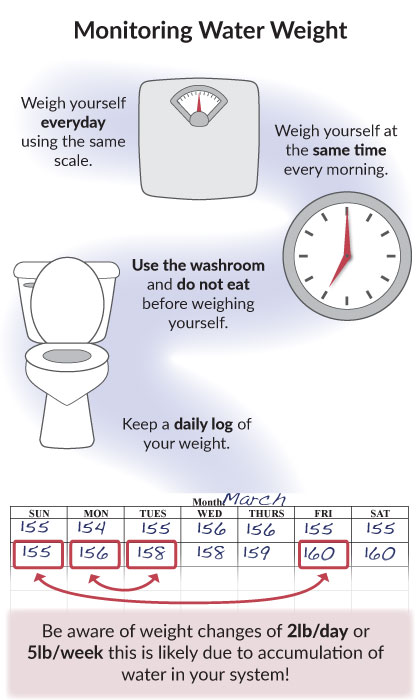
If your weight goes up by a few pounds over the course of a few days, this is not because you have gained fat or muscle. In general, changes in weight over a few days relates to accumulation of water. This may be the first sign of fluid build up. Monitoring your weight is an important way to manage your heart failure:
- You should weigh yourself every morning the same way:
- Go to the washroom and empty your bladder
- Wear the same thing every morning
- Don’t eat before weighing yourself
- Use the same scale every day
- You should record your weight on a calendar. You can use a tracking log found in the Tools section to track your weight.
What are the next steps you need to know about maintaining a fluid restriction?
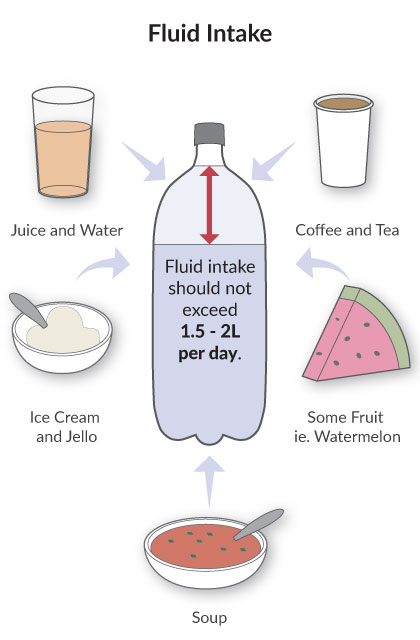
- Ask your health care provider about how much fluid you should limit yourself to each day. For patients with heart failure, this is usually 1.5 to 2 L per day. This is the equivalent of about 6 to 8 cups.
- It is important to remember that this is not just the water you drink. This includes coffee, tea, juice, soup, JELL-O, ice cream, and even some fruit (especially melons like watermelon).
Tips for Controlling Your Fluid Intake:
- Plan ahead. Spread out the fluid you drink over the day.
- At first, use a 2 L pop bottle to keep track of the fluid you are drinking. For example, when you have a cup of coffee, measure out the same amount of water, and pour it into the pop bottle. When you have filled the bottle, you have had all the fluid you are allowed for the day. You can also keep track by recording the fluid amounts on a piece of paper that you keep on the fridge.
- With a measuring cup, measure the amount of fluid held by your drinking glasses, coffee cup and soup bowl. Knowing how much fluid they hold will help you to plan the amount of fluid you can drink for the day.
- Use small cups and sip slowly.
- Take your pills with apple sauce or soft food.
- Drain excess fluid from canned fruit.
- If you are thirsty, try sucking on small amounts of hard candy or frozen grapes to help with a dry mouth. If you are diabetic, make sure the candies are sugar-free.
- Some people also find that brushing their teeth often or rinsing their mouth with chilled mouth wash helps managing thirst.
If your weight has increased, ask yourself:
- Have I consumed more salt / sodium in the last few days?
- Have I been drinking more fluid than recommended?
- Has there been a change in the amount of urine I’m producing?
Take Home Messages
- The body may lose the ability to normally eliminate extra fluid that is consumed.
- Fluid may accumulate in your legs and ankles, or in your lungs, making it difficult to breathe.
- Your health care provider will talk to you about whether you should restrict your fluid intake and the amount of the daily fluid restriction.
- Remember that your fluid limit does not just include water. It also includes coffee, tea, juices, soups (any liquids) and also some fruits that contain a lot of water (like grapes, oranges and melons).