Left Ventricular Assist Devices (LVADs) are mechanical pumps that support the main pumping chamber of the heart, the left ventricle. They are implanted in patients with advanced heart failure who are still very symptomatic despite medications and specialized pacemakers.
Unlike implantation of an ICD or CRT (which are less invasive procedures), implanting an LVAD is a major, open-heart surgery. The risk depends on how sick a patient is before the operation.
How does it work?
An LVAD is not an artificial heart. The patient’s native heart is not removed. Rather, the LVAD is attached to the patient’s heart, and is designed to take over the pumping function of the left ventricle. It takes a lot of energy to drive the pump, so although the pump itself is completely internal, a cable passes out through the abdominal wall and connects to batteries that power the pump. These batteries must be worn at all times, and require frequent recharging. Although this sounds complicated, many patients are able to adjust their lives and are often able to return to an active lifestyle.
Before the decision is made to implant an LVAD, patients undergo an extensive evaluation to make sure it is appropriate for them to undergo major surgery to implant the LVAD. This evaluation is meant to identify patients who are sick enough to need an LVAD (and justify the risk of the surgery), but not too sick to make the operation too high risk.
Currently, there are two main LVADs that are being implanted, the HeartMate II® and the HeartWare® LVAD.
Currently, most LVADs are implanted while patients await a heart transplant. This means that the patient is listed for heart transplant, but as the wait time can be long, and his/her heart is so weak, the support of an LVAD is required until a donor heart becomes available.
Other reasons For LVAD Implantation:
- In some rare cases, the cause of a person’s heart failure may be reversible and LVADs may be implanted to allow the heart to rest and recover. Once the heart has recovered, the LVAD is then taken out.
- Some patients with advanced heart failure may not be candidates for a heart transplant because of poor kidney function or high pressures in the lungs (pulmonary hypertension). Sometimes when normal circulation is returned with an LVAD, the impaired kidney function and pulmonary hypertension may improve to a point where a patient may be eligible for transplantation. Patients usually have their LVADs implanted and are then given several months to recover before they are reassessed for transplant candidacy.
- Finally, there are some patients who are not candidates for heart transplantation, and will most likely never be eligible because of age or other medical conditions (i.e. cancer, kidney failure, advanced diabetes, etc.). An LVAD may be implanted as a way to manage their severe heart failure symptoms, as a permanent solution.
Components of an LVAD
Although there are differences in the design of LVADs depending on the manufacturer, all LVADs have the following components:
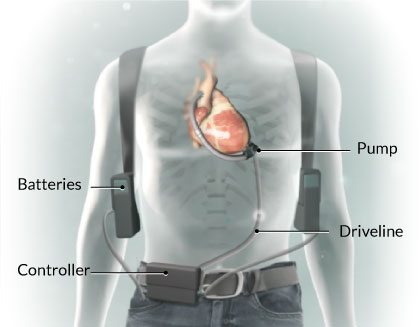
- Pump
The “workhorse” of the LVAD. This piece attaches to the left ventricle of your heart and pumps the blood to your body. A cannula empties the blood from the left ventricle and pumps it through another cannula that is implanted in the aorta. Newer generation devices do not provide a continuous pumping action so you may not be able to feel a pulse. - Driveline
This is the “power cord” of the LVAD. The LVAD requires electrical energy to run. The driveline connects the LVAD to the controller and batteries on the outside of your body. The driveline exits your body through the skin of your abdomen. - Controller
This is the “brain” of the LVAD. It records all the settings of the LVAD, tells you when the batteries need to be changed, and will alarm if there is a problem with the LVAD. The controller is worn on the outside of the body in a bag, or on your belt. - Batteries
When people are active, batteries are the main way that an LVAD is powered (it may also be powered by plugging it into an electrical power source, see below). The batteries must be charged in between use (it usually takes about 6 hours to fully charge the batteries). The controller will have a display that shows you how much battery life is left. - AC (Electrical) Power Sources
While you are at home (sleeping or resting) you can connect your LVAD to an electrical power source. This is to prevent loss of battery power while you are asleep.
Living with your LVAD
After the surgery to implant the LVAD is done, you will be in hospital for several days, and the LVAD team will follow you closely to monitor your progress. The LVAD team is composed of cardiac surgeons, cardiologists and nurse practitioners. You and your family will receive teaching on how to operate your LVAD. You will learn that your LVAD is easy to operate and very reliable.
After you go home, the LVAD team will provide you with all the equipment you need to care for your device. The LVAD will provide you with better circulation, better organ function, and will hopefully make you feeler stronger.
Commonly Asked Questions
Q: Will I be taking new medications after getting the LVAD?
After LVAD implantation, you will have different medication needs. Patients often require less medication than before surgery. Your doctor will determine which medications you will need. Most patients will need to take blood thinners while their LVAD is implanted. The nurses, nurse practitioner and pharmacist involved in your care will make sure you know each of your pills and what they do.
Q: Will I be able to shower with the LVAD?
Once your health care provider feels that your incision is healed, you will be able to shower. The nurse practitioner will show you how to cover and protect the electrical connections so that you can safely take a shower. You will not be able to swim or submerge underwater.
Q: How long can I expect to be in hospital after the LVAD is in place?
You and the LVAD team will decide when you are ready for discharge. Most patients are ready for discharge within two weeks to 1 month after surgery. It is important that you are very comfortable with the care of the LVAD.
Q: Can I have sex?
Many patients are able to resume sexual activity once the surgical wound has healed.
Q: Are there restrictions on my activities?
Like any major open-heart surgery, there is a recovery period after surgery. Over time you will regain your strength, and ideally return to an active lifestyle.
To find out more information on LVADs, visit the website, www.mylvad.com .
Take Home Messages
- Left ventricular assist devices (LVADs) are specialized mechanical pumps that take over the pumping function of the left side of the heart.
- They are often used as a “bridge” to heart transplantation.
- Implantation of an LVAD is a major open heart surgery and patients have to undergo an extensive evaluation pre-operatively.
- LVADs require a lot of energy to run, which is why they are powered by batteries that must be carried on the outside of the body at all times.