Cardiac Resynchronization Therapy (CRT), also called a Biventricular Pacemaker is a specialized pacemaker that works by making the two pumping chambers of the heart (the right and the left ventricle) pump at the same time in order to improve the overall function of the heart.
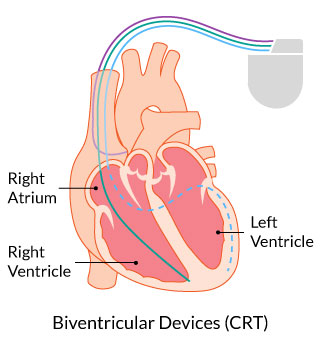
The main pumping chamber of the heart is the left ventricle. The left ventricle pumps blood to the body. The other pumping chamber is the right ventricle, which pumps blood to the lungs. In the normal heart, these two chambers pump at the same time.
In some patients with heart failure, the two ventricles lose their coordination, and the left ventricle does not pump at the same time as the right ventricle. There may be clues on your electrocardiogram, or echocardiogram, that your ventricles are not coordinated. If this is the case, your health care provider may recommend that you have a CRT device implanted to “resynchronize” the ventricles. The goal of this specialized pacemaker is to make the pumping function of your left ventricle more effective, to improve your symptoms, and make you live longer.
All CRT devices are pacemakers. If you are also a candidate for an ICD (see section on ICDs), your health care provider may recommend that you receive a combination CRT and ICD device, called a CRT-D device.
What to expect from CRT?
Several studies have shown that the majority of patients who have a CRT implanted will experience an improvement in their symptoms, including improved quality of life and exercise tolerance. Often these improvements are noted immediately after CRT implantation, but can sometimes take weeks to months to be appreciated. There is however, a group of patients who have CRT implanted who do not benefit from improved symptoms and quality of life. This subset of patients is called CRT Non-Responders. There is ongoing research trying to understand which patients are most likely to benefit from CRT.
How are CRTs implanted?
CRT implantation is usually day-surgery. They are typically implanted in the Electrophysiology (EP) Laboratory, but sometimes will be done in the Operating Room. Patients are usually awake during the procedure, and an intravenous (IV) medication is given to help you relax. With this medication, you will feel drowsy, but will be awake and able to answer questions.
Most CRTs are implanted using the transvenous approach. Freezing solution is injected under the collarbone, and a small incision is made. The wire (or wires) are then inserted through the incision into a vein and are then directed to the heart using X-Ray guidance. The tip of the wire is attached to the heart muscle, and the other end is hooked up to the pulse generator. The generator is then implanted under the skin just under the collarbone.
The procedure usually takes between 2 and 4 hours.
After CRT implantation, you will be given information about your specific device. You will also receive a follow-up appointment in the Device Clinic for ongoing monitoring of your CRT.
What are the risks of CRT?
In general, CRT implantation is safe, however, as with any invasive procedure, there are risks. The doctor who performs the procedure will talk to you more about the risks, and ask you to sign a consent form if you agree to go ahead with the procedure.
In general, the risks of CRT implantation are similar to those associated with any other type of pacemaker implant. These include bleeding, infection, puncture of the lung requiring a chest tube and damage to the heart or to a blood vessel. Overall the risk of having any of these complications is about 2 to 3%. The risk of dying from a CRT implantation procedure is very low and is less than 1%.