Hypertrophic cardiomyopathy (HCM) is a condition where the heart muscle becomes abnormally thickened. There are other reasons that the heart muscle can become thickened – most commonly it is because of having high blood pressure for many years. In hypertrophic cardiomyopathy, the thick heart muscle is because of a genetic mutation. This means that it can run in families.
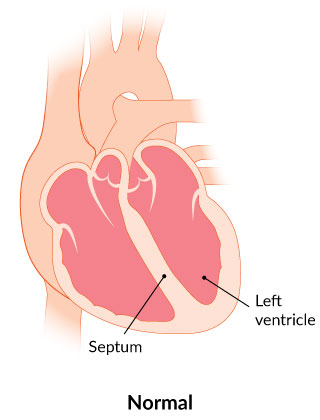
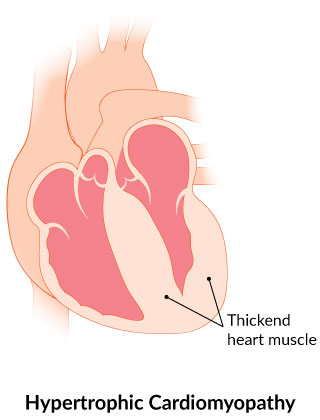
Sometimes the thickened heart muscle can block blood flow out of the heart. In this case, it is called hypertrophic obstructive cardiomyopathy (HOCM).
Because the heart muscle is thick, the heart doesn’t relax well, so people with hypertrophic cardiomyopathy can have symptoms of heart failure. They may also experience dizziness, chest pain, shortness of breath, palpitations (racing heart) or fainting.
Hypertrophic cardiomyopathy is also the most common reason for sudden death in a young person. After being diagnosed, people with hypertrophic cardiomyopathy should not participate in competitive sports.
Sometimes fainting can be because of ventricular arrhythmias (abnormal fast rhythms from the bottom chamber of the heart). In this case, an implantable cardioverter defibrillator (ICD) may be considered (see section on ICD).
If a family member is diagnosed with hypertrophic cardiomyopathy, other individuals in the family should be screened. Tests to screen for hypertrophic cardiomyopathy include an echocardiogram or a blood test to look for a genetic mutation.
Depending on the severity of the disease, a number of therapies are available. These include medications, invasive procedures (like septal alcohol ablation or surgical myectomy) and devices (like an ICD). Sometimes the disease is so severe that people may be considered for a heart transplant.