Atrial fibrillation is a problem with the electrical system of the heart. The electrical system is different from the arteries around the heart, so it is not the same thing as coronary artery disease, or a heart attack.
The signal for the heart to beat is based on electrical activity. This electrical activity usually starts in the upper chambers of the heart (the atria) and is communicated to the bottom chambers (the ventricles), which tells them to contract.
In the normal situation, the atria and ventricles work together. The atria contract and send blood to the ventricles, which in turn contract and send blood to the lungs and the body.
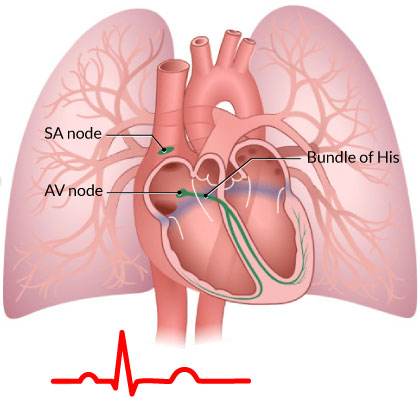
The sinus node (or SA node) is a small group of specialized cells in the top part of the right atrium that acts as the body’s natural pacemaker. It sets your heart rate. When you exercise, or are excited, it fires faster, causing a faster heart rate. When you are relaxed or are sleeping, it fires more slowly, resulting in a slower heart rate.
The electrical signal is then sent to the AV node, which is another specialized group of cells in the middle of the heart between the atria and the ventricles. This then transmits the signal to the ventricles (through the Bundle of His), telling them to contract. When the sinus node is regulating the heart’s contraction, this is called sinus rhythm.
In atrial fibrillation, instead of there being one electrical signal being sent from the sinus node to the AV node, there is disorganized, chaotic electric activity in the atria. This causes the atria to beat irregularly and quickly, to “fibrillate”. This sends several signals to the AV node, which in turn causes the ventricles to beat quickly and irregularly.
How Common is Atrial Fibrillation?
Atrial fibrillation is the most common cardiac arrhythmia (abnormal heart rhythm), and affects about 350,000 Canadians. Atrial fibrillation becomes more common as we age. Approximately 10% of Canadians over the age of 80 have atrial fibrillation.
What Causes Atrial Fibrillation?
There are many risk factors for atrial fibrillation. The most common include older age, and having high blood pressure for many years. Other risk factors include being overweight, having sleep apnea, and having abnormalities of the thyroid function. There is also likely a contribution of genetics, which we are learning more about.
What is the risk with Atrial Fibrillation?
There are two main problems with having atrial fibrillation:
- Firstly, because there is disorganized electrical activity in the atria, there are many electrical signals sent to the ventricles. This can cause the heart to beat quickly and irregularly. If the heart rate is very fast, patients may experience palpitations, or may feel fatigued or lightheaded. Most people with atrial fibrillation are unaware of the irregular heartbeat. Medications can be used to control this fast heart rate (see below).
- The other potentially devastating consequence of atrial fibrillation is having a stroke. Because the atria are “fibrillating”, blood pools. When blood pools, a blood clot may form. If this blood clot is pumped to the brain, it causes a stroke. It is estimated that about 20% of strokes are caused by atrial fibrillation. Unfortunately, the strokes associated with atrial fibrillation tend to be large strokes and often leave patients with significant disability (like not being able to move half your body, being unable to speak or look after your self). Blood thinners can reduce the risk of having a stroke (see below).
How is Atrial Fibrillation Diagnosed?
Atrial fibrillation is diagnosed with an ECG, however, may also be detected with a heart monitor that you wear for a longer period of time (like a holter monitor or loop recorder). Sometimes these tests are ordered after an individual has a stroke to see if atrial fibrillation has caused the stroke.
After atrial fibrillation is diagnosed, other tests are usually considered. An echocardiogram (ultrasound of the heart) is usually ordered to make sure that there is not an underlying structural problem with the heart (like a weak heart muscle or valve problem). A blood test to check the thyroid function is also usually ordered.
Other tests, like a sleep study, may be considered see if sleep apnea is contributing to the atrial fibrillation.
Are there different types of Atrial Fibrillation?
Yes, sometimes people may be in atrial fibrillation for a period of time and then naturally go back to normal heart rhythm (called sinus rhythm). This is called paroxysmal atrial fibrillation.
Other people are in atrial fibrillation all of the time. This is called permanent atrial fibrillation.
How is Atrial Fibrillation treated?
There are a number of ways that atrial fibrillation can be treated, including medications, and procedures. The goal of treatment is to reduce the symptoms of atrial fibrillation, control the heart rate and to prevent a stroke.
- Electrical Cardioversion – This involves shocking the heart to put it back into the normal rhythm. This is normally done as a day procedure. The patient is put to sleep briefly and an electrical shock is delivered to the heart.
- Medications to control the heart rate – These include beta-blockers, calcium channel blocks and digoxin. These medications slow the heart rate but do not put the heart back into the normal rhythm.
- Medications to maintain sinus rhythm – Sometimes medications, called anti-arrhythmics, are used to try to maintain the heart in the normal rhythm (sinus rhythm).
- Ablation – This is an invasive procedure, where catheters (or tubes) are inserted in the groin and passed to the heart. Small areas of the heart that are thought to be responsible for the atrial fibrillation are then destroyed with these tubes.
- Blood thinners – Blood thinners are used to reduce the risk of stroke in patients with atrial fibrillation (see below for more information)
What blood thinners available?
There are a number of different options for blood thinners to lower the risk of stroke in atrial fibrillation.
If one is required, and which blood thinner is recommended depends on an individual’s risk of stroke. In people who are at a very low risk of having a stroke, no blood thinner may be necessary. Most people, however, require a blood thinner.
Aspirin is a mild blood thinner, and lowers the risk of stroke in atrial fibrillation by about 20%.
There are more powerful blood thinners that reduce the risk of stroke even further, up to 60-70%.
Warfarin, or Coumadin, is an older medication that has been used for many years, and is effective at preventing strokes. It is however, not an easy medication to take as there is not one dose for everyone, and individual’s dose will usually change over time. Regular blood test (called an INR) is required to make sure the blood is thin enough, but not too thin. Warfarin also has a lot of interactions with other medications and some foods.
There are newer medications that have been shown to be as effective as warfarin in reducing the risk of stroke, and have the advantage that they do not require blood tests to monitor. These are called direct oral anticoagulants, and there are currently three available in Canada:
- Dabigatran (Pradaxa®)
- Rivaroxaban (Xarelto®)
- Apixaban (Eliquis®)
These medications are all cleared by the kindeys, so they can’t be used in people with reduced kidney function. They are also not safe in patients with mechanical heart valves.
What are the downsides of being on a blood thinner?
The main downside of being on a blood thinner is the risk of bleeding. If you are on a blood thinner and hit yourself, you will bruise more easily. If you cut yourself, it will take longer to stop bleeding. This type of minor bleeding is not a big concern.
The main concern is major internal bleeding – usually in the gastrointestinal tract (stomach or colon). It will be obvious if you see red blood in your bowel movement that you are bleeding internally. However, if the bleeding is coming from the stomach, by the time is works it way down, it may come out in the bowel movement as a dark black tar. If you notice anything like this, you should immediately seek medical attention.
The other main site of internal bleeding is inside the brain. This is very rare, but can be devastating. It may occur after trauma (like a fall) or sometimes spontaneously. Slurred speech or drowsiness may be a sign of this complication, and requires immediate medical attention.
There are reversal agents (antidotes) being developed for all of the blood thinners mentioned above.
Your healthcare provider will talk to you about which blood thinner option is best for you.