Pediatric Liver transplant: Living donor left lateral segment
Recipient procedure
00:08 SURGICAL PLANNING
01:42 Exposure & mobilization
02:16 Portal dissection
04:16 Mobilization of liver from inferior vena cava
05:02 Liver isolation & extraction
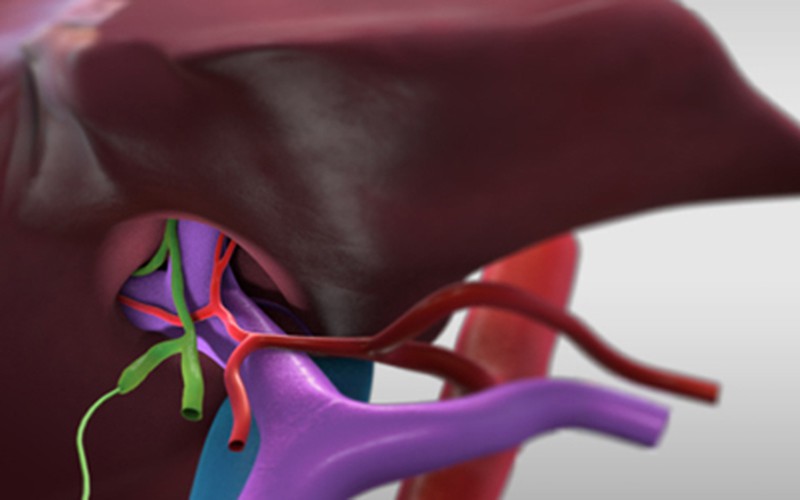
06:18 Backbench: preparation of left lateral donor graft
06:54 IMPLANTATION
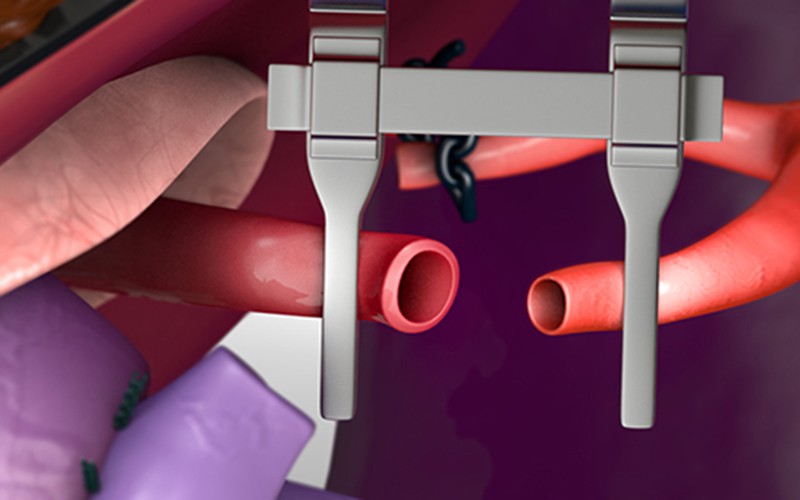
08:23 Portal vein anastomosis
11:37 Hepatic artery anastomosis via surgical microscopes
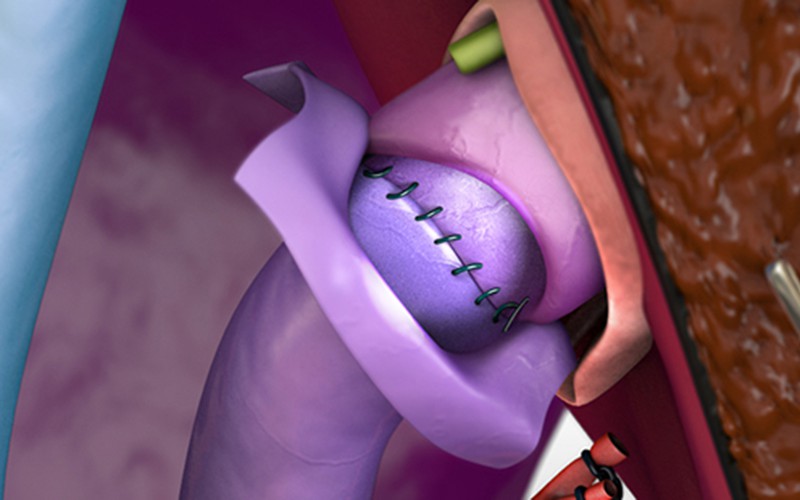
12:27 Roux-en-Y hepaticojejunostomy
14:06 Closure
Case description
- The patient is a 5 year old female with citrullinemia who suffered from frequent hospital admissions due to hyperammonemic encephalopathy.
- Aside from the metabolic defect associated with this disorder, the patient's native liver function is otherwise normal, without portal hypertension or cirrhosis.
- The graft was procured from the patient's father, and consists of segments II and III, and a portion of segment IV.
- In pediatric liver transplantation, the frequent use of partial liver grafts, smaller blood vessel diameter, donor-recipient size mismatch and challenging anastomotic orientation all contribute to a significant rate of vascular complications, compromising graft and patient survival.
- A recent review of the Studies of Pediatric Liver Transplantation (SPLiT) Registry dataset revealed that our centre had the lowest incidence of vascular complications in North America (Englesbe MJ et al. AJT 2012; 12(9): 2301-6).
- In this video of a living donor left lateral segment transplant, the graft type associated with the highest risk of vascular complications, we highlight techniques of vascular reconstruction that have been associated with low complication rates.
References
CT scans (recipient post-op)
Click to turn annotations on/off
CT scans (donor pre-op)
Click to turn annotations on/off