Management of Postpartum Hemorrhage (PPH)
00:08 Definition and Etiologies
01:39 Prevention of PPH
02:44 Management of PPH
04:04 Medical management
05:00 Uterine compression: non-surgical
07:58 Uterine compression: surgical
10:56 Surgical management
12:47 Interventional radiology
Definitions of PPH
- Primary PPH is defined as excessive bleeding within the first 24 hours of birth
- Secondary PPH occurs after 24 hours and up to 6 weeks postpartum.
- Blood flow to the uterus at term is estimated at 500ml/min. The primary mechanism at controlling blood loss postpartum is uterine contraction.
- Complications of PPH include
- iron deficiency anemia
- exposure to blood products
- coagulopathy
- shock with associated organ damage
- pituitary infarction (Sheehan’s syndrome)
- admission to the intensive care unit
- death
Etiologies
- Uterine tone can be suboptimal in context of atony or bladder distention. Polyhydramnios, multiple gestation, macrosomia, rapid labour, prolonged labor, advanced parity, prolonged augmentation, chorioamnionitis, uterine anomalies including fibroids, and nitroglycerin use can contribute to decreased uterine tone.
- Retained tissue can include products of conception including succenturiate lobe or abnormal placentation, as well as retained blood clots from an atonic uterus. Risk factors include incomplete delivery of placenta, abnormal placentation, previous uterine surgery, and advanced parity.
- Trauma of the genital tract can include vaginal, cervical, and/or uterine injury such as lacerations, extensions, uterine rupture and/or uterine inversion. Risk factors include precipitous delivery, operative delivery, fetal malposition, impacted fetal head, previous uterine surgery, and advanced parity.
- Thrombin includes pre-existing or acquired coagulopathy. Hereditary risk factors include hemophilia A, Von Willebrand’s disease, and history of previous postpartum hemorrhage. Acquired risk factors include therapeutic anticoagulation, idiopathic thrombocytopenia purpura, pre-eclampsia, disseminated intravascular coagulation, placental abruption, chorioamnionitis, amniotic fluid embolus, and fetal demise.
Medical management
OXYTOCIN
- Oxytocin is considered a first-line agent in prevention and management of postpartum hemorrhage. Oxytocin triggers increases in intracellular calcium levels in uterine myofibrils which stimulate contractions.
- In low-risk vaginal deliveries, oxytocin should be administered routinely by intramuscular (10 IU) injection at delivery of the anterior shoulder.
- An IV bolus over 1-2 minutes of 5 IU oxytocin can be used following vaginal delivery in the context of postpartum hemorrhage but is not recommended with elective caesarean section at this time.
- Intravenous infusion of oxytocin (20-40 IU in 1000mL, running at 125-150mL per hour) is an acceptable alternative or adjunct to the intramuscular injection.
- Potential risks of oxytocin include hypotension and water intoxication.
CARBETOCIN
- Carbetocin is a long-acting oxytocin which is given as a 100 microgram IV bolus over one minute. It is recommended following elective caesarean section and following vaginal deliveries with risk factors for postpartum hemorrhage as studies have shown it reduces bleeding and decreases the need for therapeutic uterotonics compared to a continuous infusion of oxytocin.
SECOND-LINE UTEROTONIC AGENTS
- Second-line uterotonic agents include ergonovine, carboprost, and misoprostol.
- Ergonovine (also known as Ergometrine) is an ergot alkaloid that primarily affects uterine smooth muscle to stimulate sustained contractions. Ergonovine is administered as 0.25mg IM or IV and can be repeated once at fifteen minutes then every two hours to a maximum of five doses. Ergonovine is contraindicated in people with hypertension and people currently managed with protease inhibitors.
- Carboprost (also known as Hemabate) is a synthetic prostaglandin analogue of PGF2 alpha with oxytocic properties that promote uterine contractility. Carboprost is administered as 0.25mg IM and can be repeated every fifteen minutes to a maximum of eight doses (2mg). Carboprost is contraindicated in patients with asthma as it can induce bronchospasm.
- Misoprostol is a synthetic prostaglandin E1 analog that binds to myometrial cells to cause strong myometrial contractions. Misoprostol is administered as 600-800 micrograms by oral, sublingual, vaginal or rectal route. The time to peak concentration is shorter with oral or sublingual administration, however the side effects of pyrexia and gastrointestinal upset are more common. Vaginal or rectal dosing have slower onset of effects, but they remain for a longer duration.
- A frequently used adjunct medication in cases of obstetric hemorrhage is tranexamic acid. The pivotal role of fibrinogen and hyperfibrinolysis in postpartum hemorrhage is increasingly recognized. Tranexamic acid (also known as Cyklokapron) is a potent inhibitor of fibrinolysis and in a study of patients with postpartum hemorrhage, administration reduced mortality due to bleeding by 19%. Therefore, it is recommended that tranexamic acid (1g IV) be administered within three hours of birth in addition to standard care for people with postpartum hemorrhage.
Uterine compression
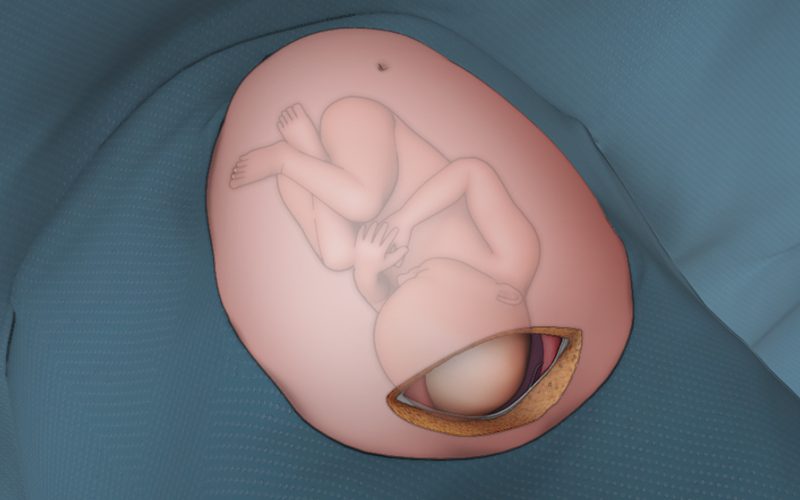
- Two commonly used techniques for non-surgical uterine compression are: Bimanual uterine compression/massage and intrauterine balloon.
- Contraindications to intrauterine balloon placement include cervical cancer, purulent infections of the vagina, cervix or uterus, untreated uterine anomaly, or in cases of arterial bleeding or disseminated intravascular coagulation requiring surgical exploration or angiographic embolization.
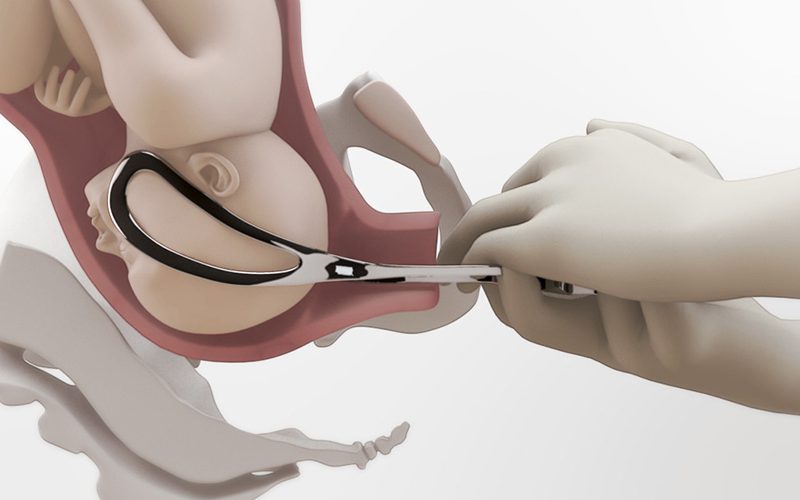
- Surgical unterine compression uses compression sutures like, modified B-Lynch suture and Cho square suture to apply external pressure on the uterus and myometrial vessels.
Surgical management
- For intractable PPH, ligation of the uterine or internal iliac arteries should be considered.
These techniques mitigate bleeding by decreasing uterine artery pulse pressure. - In the case of ongoing intractable hemorrhage, hysterectomy may be indicated.
Interventional radiology
- When available, uterine artery embolization can be an effective technique to block blood supply and control heavy bleeding.
- The patient must be stable enough for transfer to the Interventional Radiology suite.