Ante situm hepatic vein and caval reconstruction
With in situ cold perfusion of the liver for IVC stenosis and Budd Chiari Syndrome
00:08 SURGICAL PLANNING
02:44 Mobilization & caudate resection
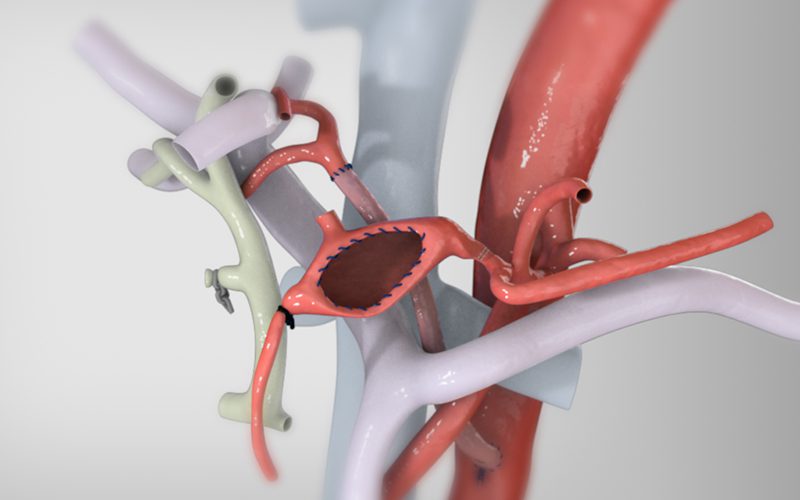
05:07 In situ cold perfusion and resection of the IVC
Case Description
- The patient was a 24-year-old female with Membranous Obstruction of the Vena Cava (MOVC).
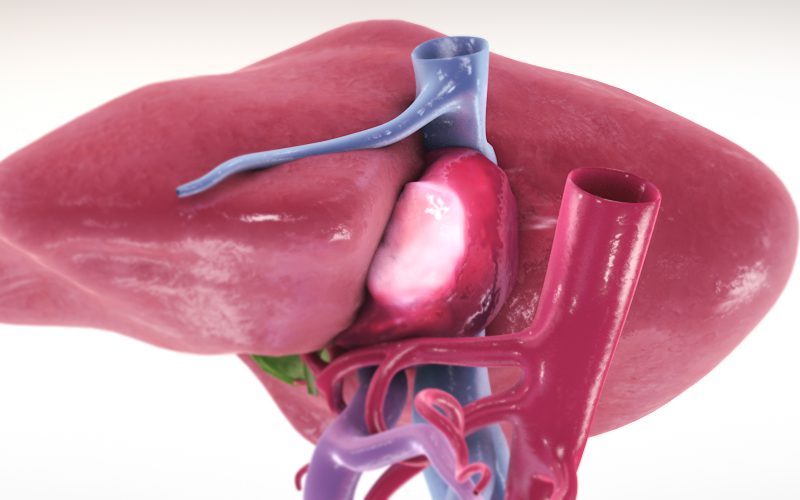
- MOVC is a rare condition characterized by progressive stenosis of the retrohepatic inferior vena cava (IVC) which can result in hepatic vein outflow obstruction and chronic Budd-Chiari Syndrome (BCS).
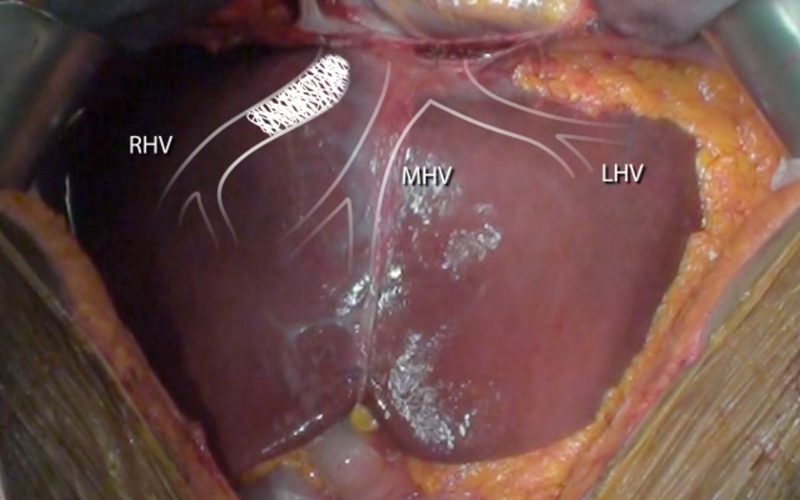
- The sub diaphragmatic IVC, right, and middle/left hepatic vein were tightly stenotic.
- The right lobe was drained via a large segment 6/7 venous branch and a large intrahepatic collateral crossing vein. The left lobe was drained via the left phrenic vein.
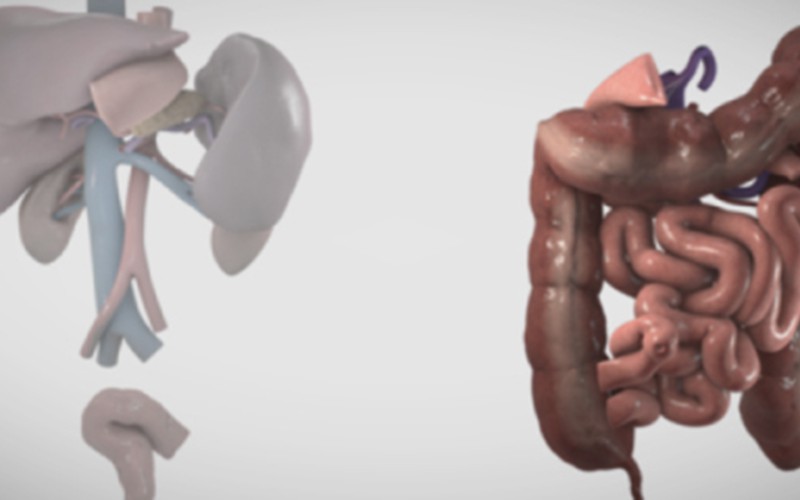
- A hepatic ante situm technique (full mobilization of the liver with transection of the suprahepatic and infrahepatic vena cava, followed by rotation of the liver so that the vena cava and hepatic veins are anterior and accessible) combined with hypothermic in situ perfusion of the liver was chosen as the most optimal surgical approach.
- Hypothermic perfusion allows the liver to be maintained without blood flow for more than one hour without significant parenchymal damage.
CT scans (Pre-RHV stent insertion)
Click to turn annotations on/off
CT scans (Post-RHV stent insertion)
Click to turn annotations on/off
CT scans (Narrowed RHV stent)
Click to turn annotations on/off