Anterolateral Thigh Perforator Flap Harvest
Subfascial harvesting technique
00:10 Surgical planning
03:55 Exposure
06:11 Perforator dissection
08:28 Descending branch dissection
11:53 Harvest & Closure
- The anterolateral thigh flap involves the skin paddle, the descending branch pedicle of the lateral circumflex femoral artery, and the perforators to the skin paddle.
- The descending branch pedicle is situated between the rectus femoris and vastus lateralis muscle.
- The major perforators to the skin paddle are normally located within a 2 to 3 cm radius from the midpoint between the anterior superior iliac spine and lateral border of the patella.
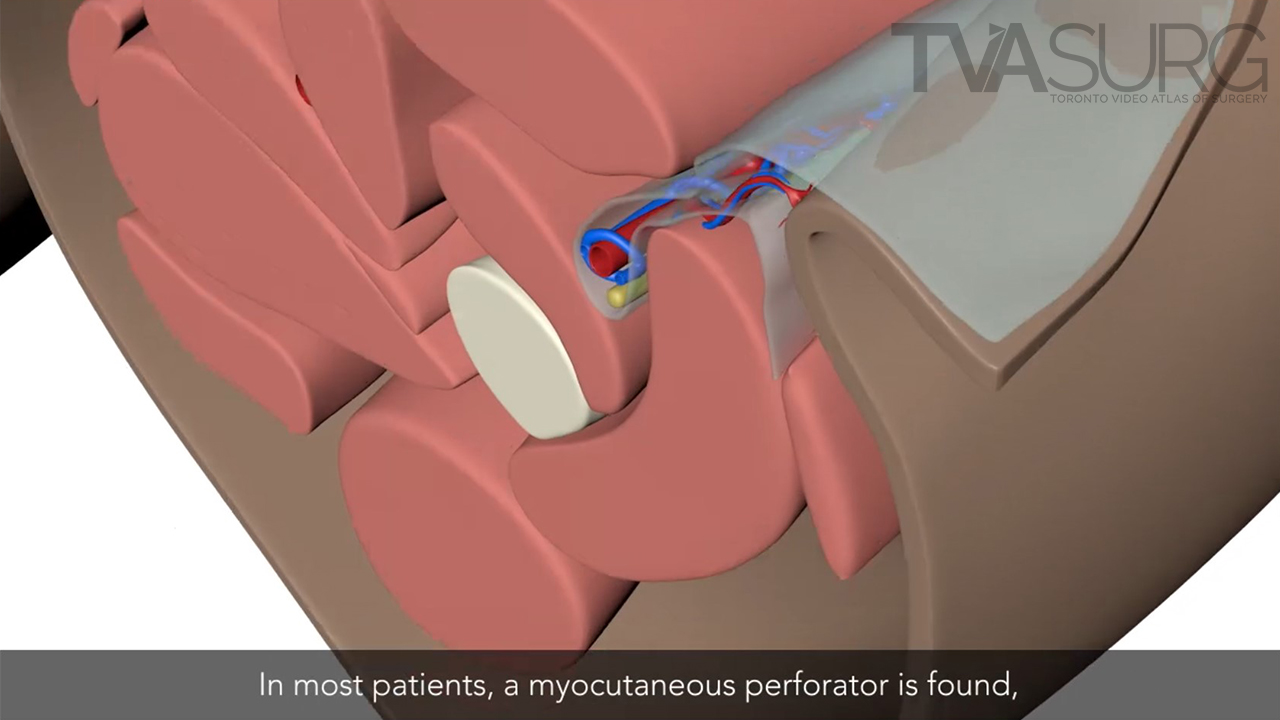
- In this unique case, both myocutaneous and septocutaneous perforators are present. More commonly, only a myocutaneous perforator is found, which traverses the medial edge of the vastus lateralis muscle.
- The vastus lateralis muscle is dissected to free the myocutaneous perforator. A small muscle cuff is left beneath the perforator to identify the orientation and prevent twisting and injury to the perforator.
- The pedicle is divided distal to the perforators. On the proximal end, the pedicle is divided distal to the branch to the rectus femoris muscle, preserving the blood supply to this muscle.
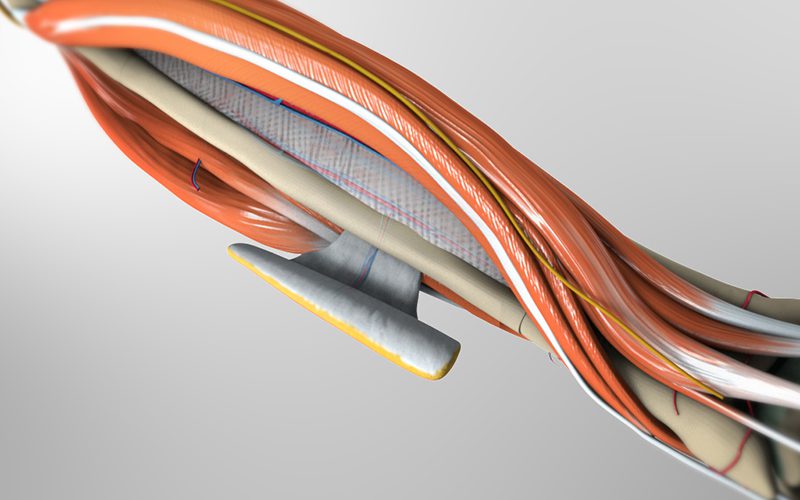
- The subfascial harvesting technique dissecting the plane below the fascia lata, taking the fascia with the flap. The fascia is carefully transected to maintain a safe distance of 2 to 3 cm to the perforators.
- Care is taken to spare the motor branch of the femoral nerve to the vastus lateralis muscle during dissection.
** Please buy pro to create nested accordion** id="14603"]
Here are a few key moments from the production of this video.
Video editing was done in Adobe Premiere Pro. For this case we had multiple cameras set up in the OR at various angles, to ensure we captured all the important steps of the case.
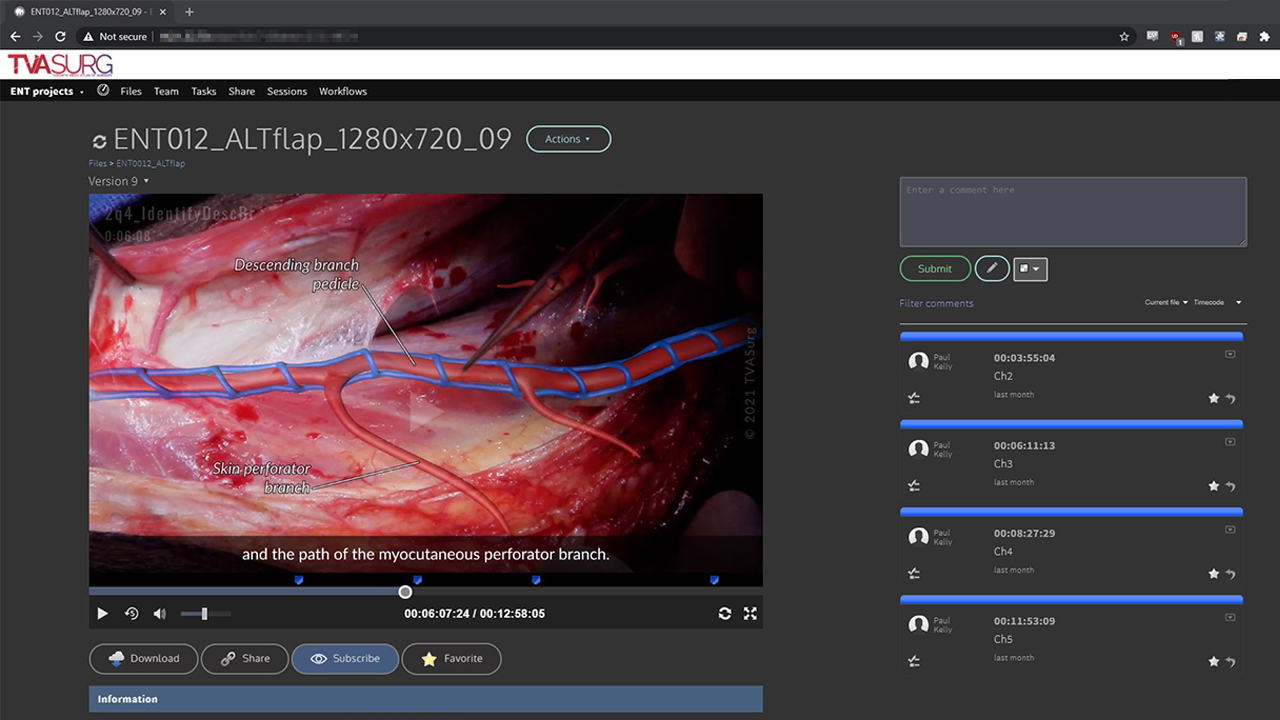
As the video is developed, we use a video review system called Kollaborate to share updates with our surgeon editors. This allows them to see the progress on a video and share comments, which are time-stamped to the video draft.
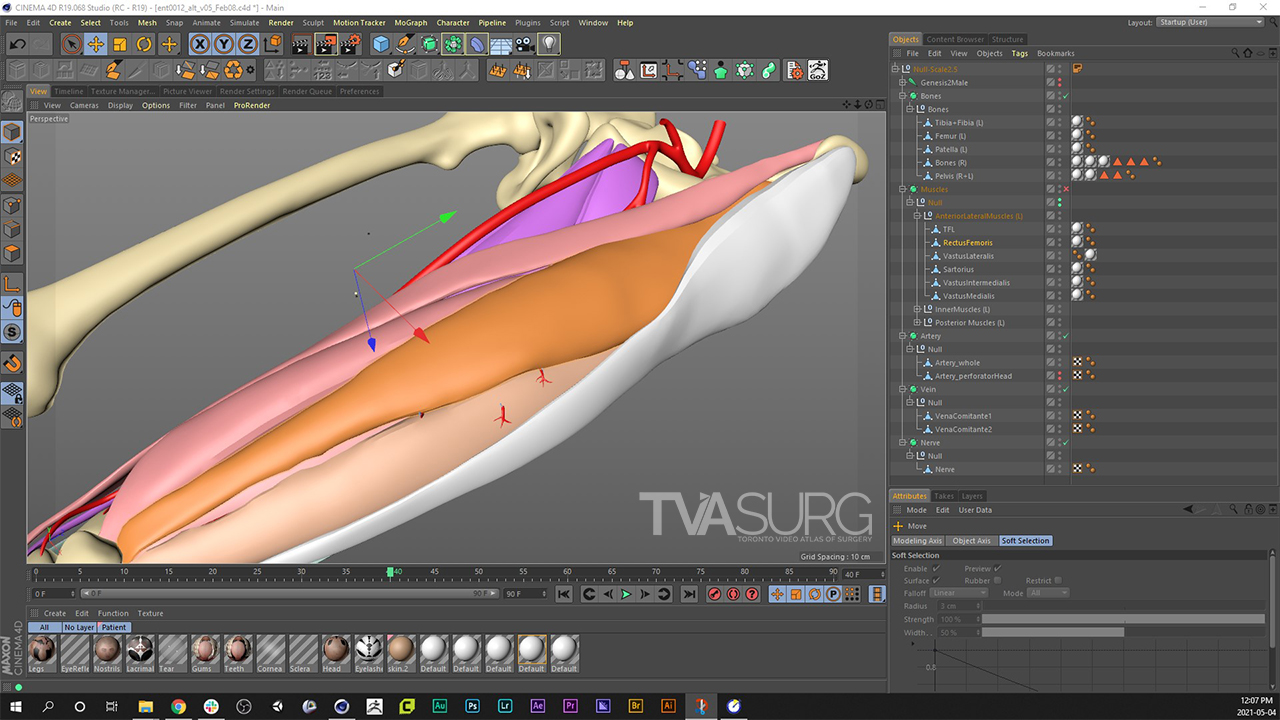
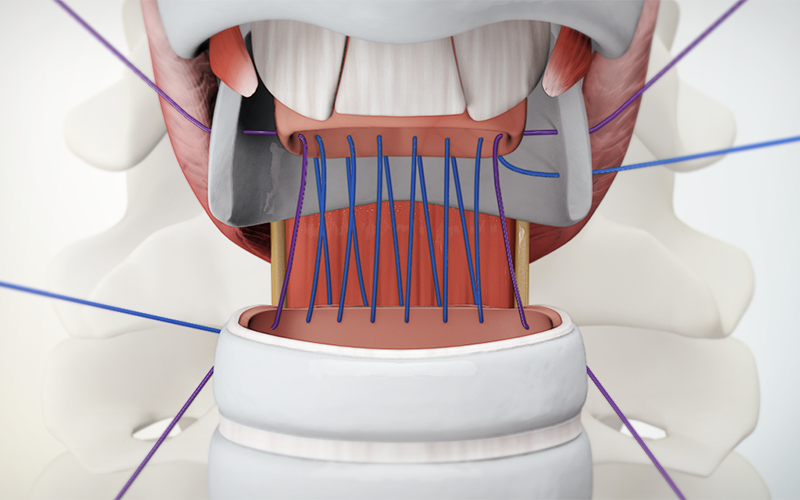
We create and refine the base models in our animation software, Cinema4D.
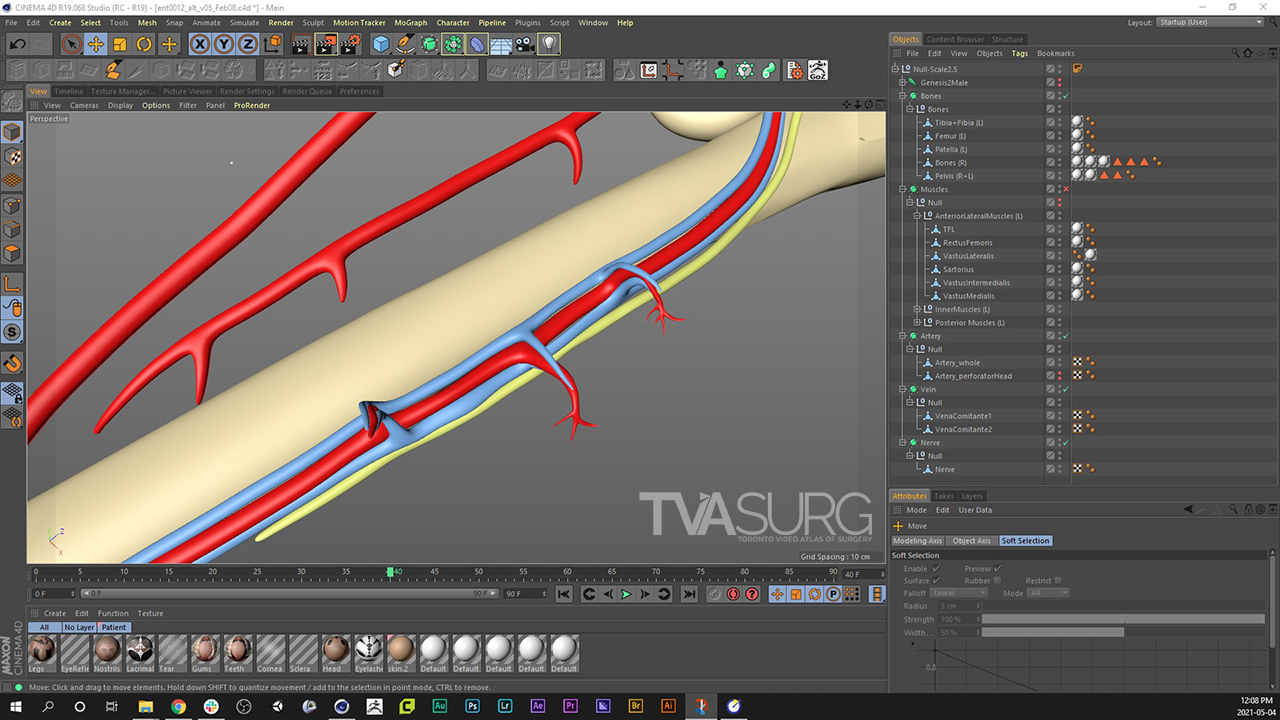
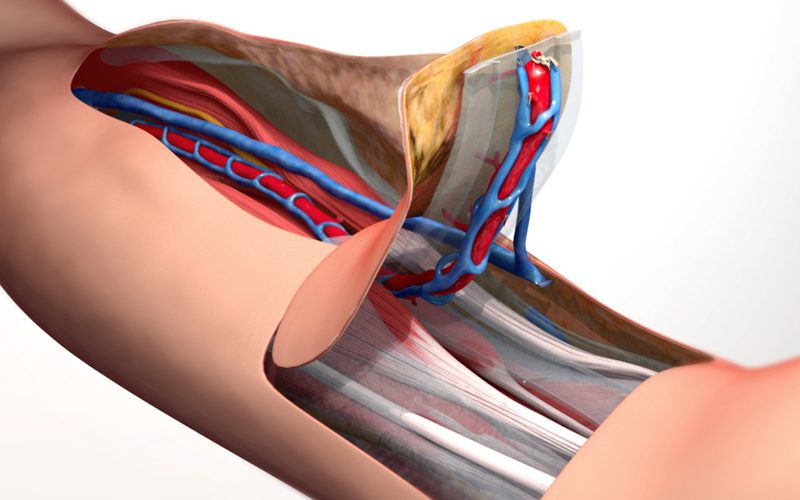
In many surgical procedures we have to depict esoteric structures that you aren't likely to find on stock models, so these are often custom modelled on a case-by-case basis. Here we've modelled the myocutaneous and septocutaneous branches of the descending branch pedicle, which supply the skin island portion of the flap.
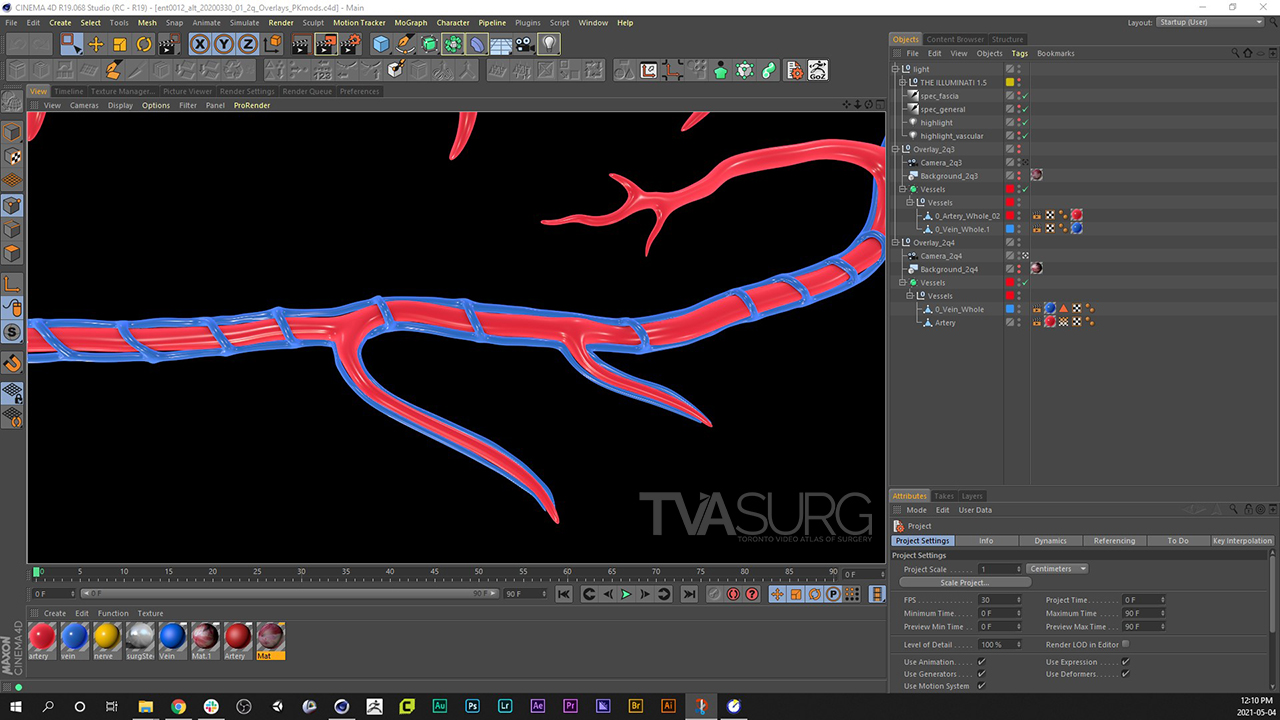
The black background in the rendered image indicates areas where the pixels have no RGB value, so will appear as transparent when composited with other images or footage.
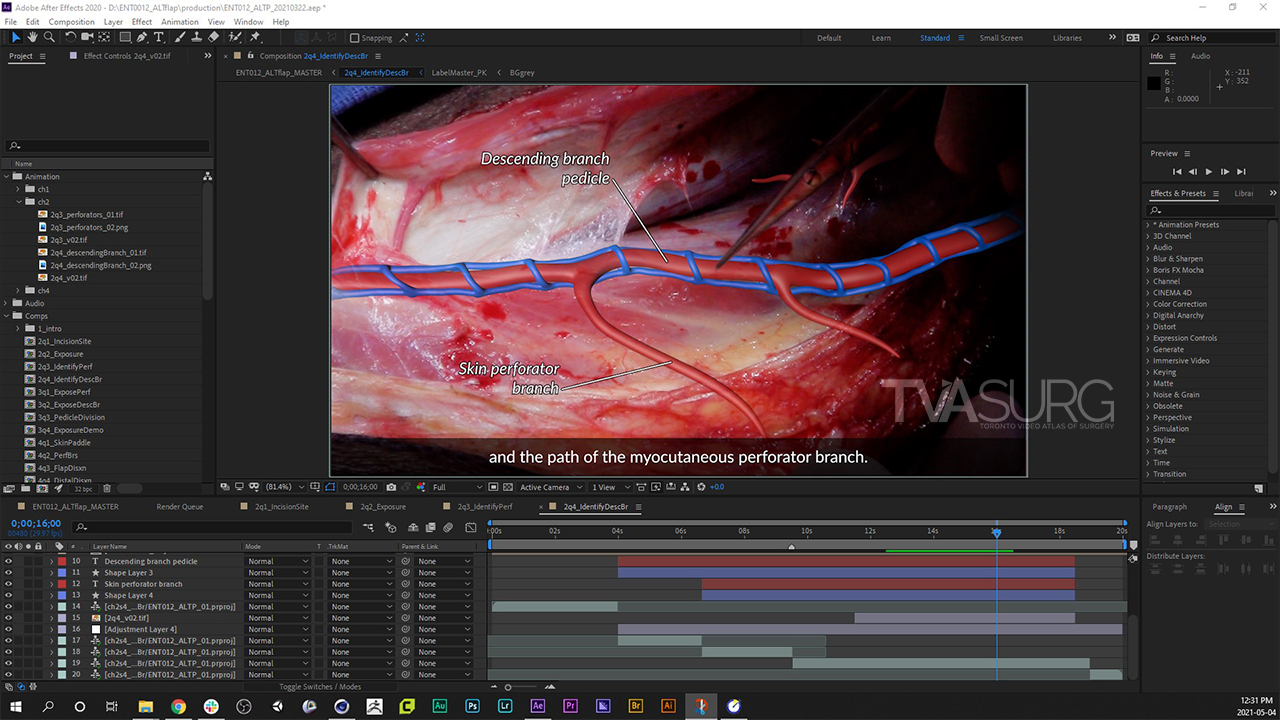
Using a render with a transparent background, we can also use masking and opacity adjustments to overlay an illustration over live footage, giving the audience a clear understanding of the anatomy present, which in some cases may be difficult to discern from surrounding tissues of similar appearance, or may be deep to what is shown at that moment.
During the review process we create animation "playblasts", which are screen-recordings of the animation software viewport without scene lighting or surface textures applied.
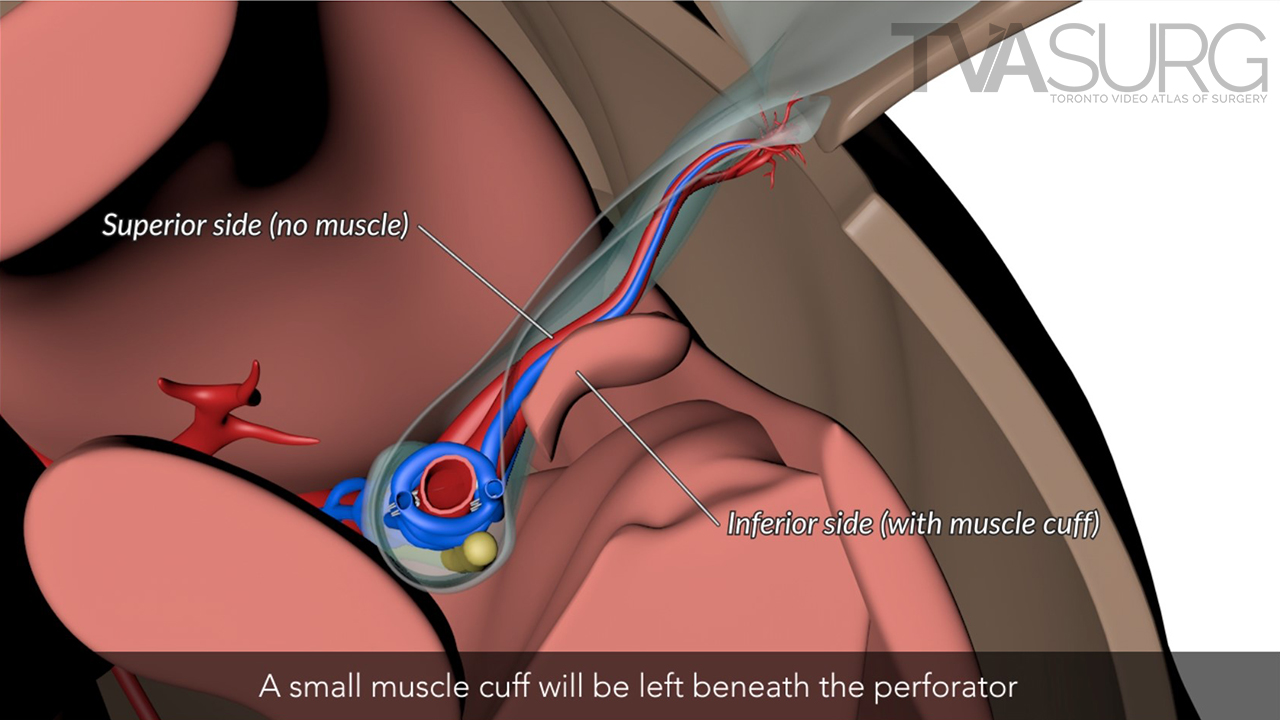
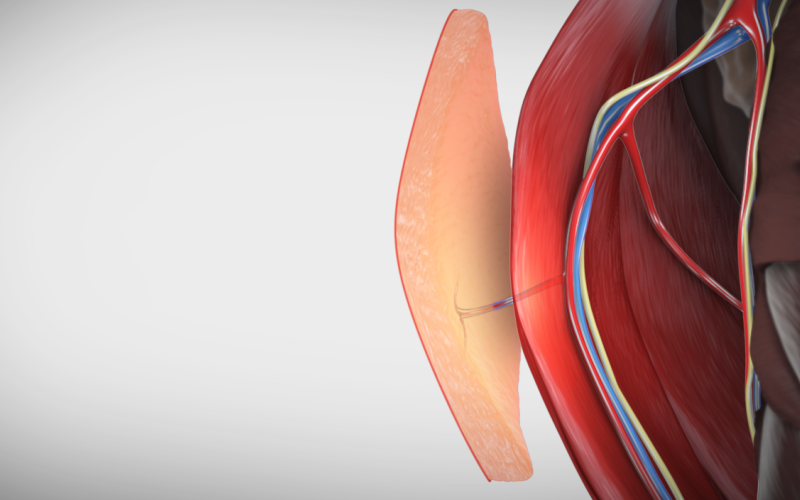
In this case we used cross-sectional anatomy to depict certain structures that were difficult to appreciate from a straight-on view, due to their depth relationships.
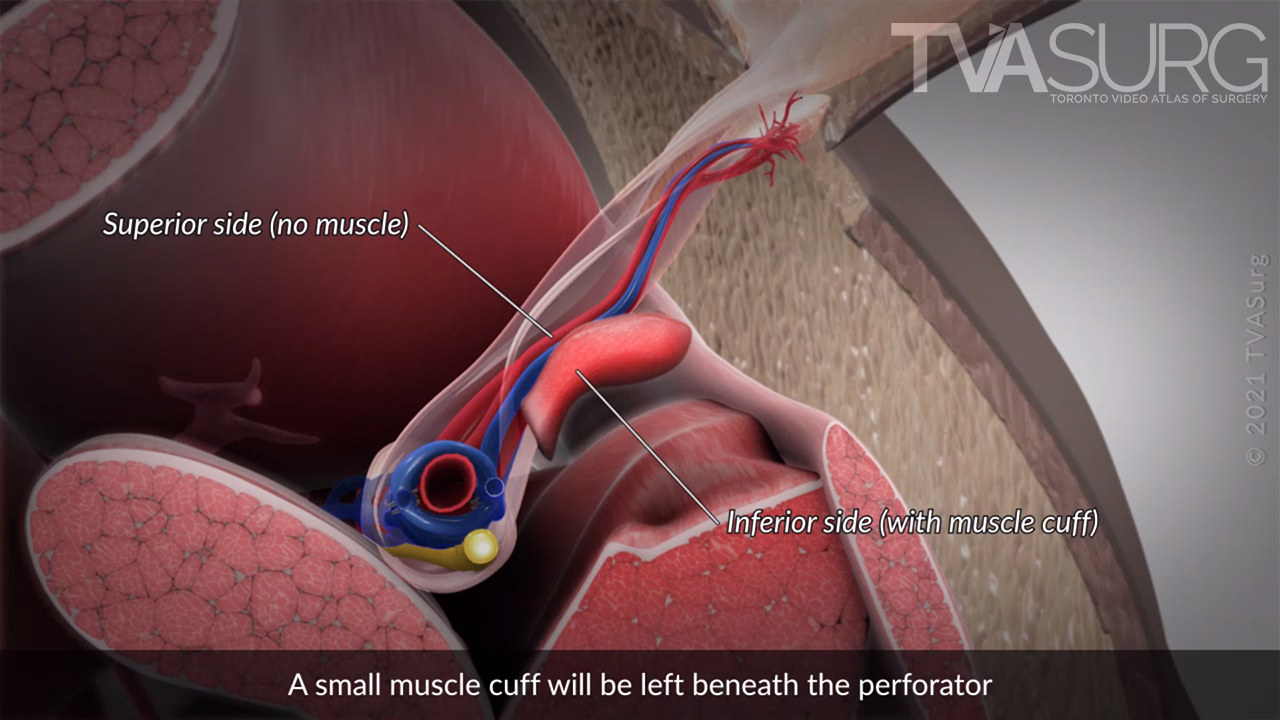
In the final stage of production, we render out the animation shots in high-quality, with tissue-specific textures and cinematic lighting.